Cardiovascular Risk Management Must Always Consider Social Determinants of Health: Past Lessons, Data, Proposals and Challenges
Salinas AM and Kones R
DOI10.21767/2572-5483.100035
1Cardiocentro Ernesto Che Guevara, Villa Clara, Cuba
2Medical Director, Cardio-metabolic Research Institute Houston, Texas, USA
- *Corresponding Author:
- Salinas AM
Cardiocentro Ernesto Che Guevara
Villa Clara, Cuba
Tel: +5342225342
E-mail: cardioams@yahoo.es
Received date: March 20, 2018; Accepted date: May 18, 2018; Published date: May 25, 2018
Citation: Salinas AM, Kones R (2018) Cardiovascular Risk Management Must Always Consider Social Determinants of Health: Past Lessons, Data, Proposals and Challenges. J Prev Med Vol.3 No.2: 14.
Copyright: ©2018 Salinas AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Traditionally, management of cardiovascular risk (CVR) has been focused on clinical factors, and this approach has advanced cardiology and improved patient outcomes for decades. Nevertheless, CVR is influenced by biological, psychological, economic, and environmental elements, as well by health systems. The broader background concerning the social determinants of health (SDH) and socioeconomic status (SES), a major component of SDH, upon noncommunicable diseases and CVR in particular has recently been reviewed in detail elsewhere.
Keywords
Cardiovascular risk; Obesity; Hypercholesterolemia
Cuban Deprivation during the “Special Period”: 1988-1994
Unwitting experiments of nature and fortune, particularly the ravages of war and political changes, create circumstances that would otherwise be unethical to produce. Study of such unusual conditions is warranted, since they may inform concepts that have applications when order is restored and conditions are stable.
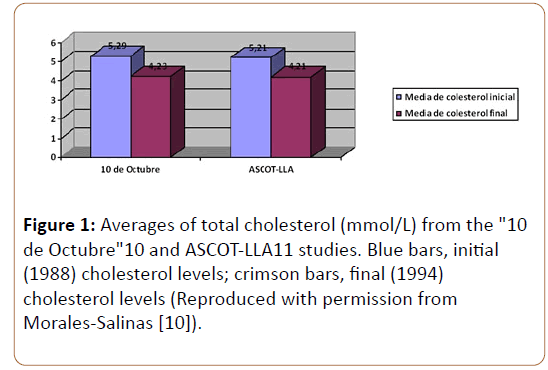
An outstanding example from Cuba concerns the relationship between SES and CVR. After a period of decline, the USSR dissolved in 1991; it was a major trading partner with Cuba and a prominent member of the Counsel of Mutual Economic Help (CAME, for its acronym in Spanish) of the socialist countries [1-10]. This sudden absence of support began a “Special Period” in Cuba, characterized by a severe shortage of oil, transportation, electricity, and food. The famine that followed involved a marked reduction in consumption of animal protein, a corresponding increase in plant food intake, and a rise in physical activity (walking, bicycling) in the general population. In a cohort that randomly measured CVR factors before (1988) and during (1994) the Cuban Special Period in the 1990s, there was a dramatic decrease in sedentary lifestyle, obesity, hypercholesterolemia, diabetes, and tobacco use (Table 1 and Figure 1) [5]. Attention is called to two features: (i) the fall in mean cholesterol levels was on the order of the therapeutic effect of statin drugs [11] and (ii) of all modifiable risk factors, blood pressure was the only one to rise during the same period [10]. In practice, this descriptive research was a quasiexperimental study of the health effects of the unexpected intervention of the severe socioeconomic crisis endured by the Cuban people.
| Risk factor | Prevalence in 1988 (n=3011) | Prevalence in 1994 (n=2535) | Percentage change |
|---|---|---|---|
| Per capita calorie consumption (kcal/day) | 2899 | 1863 | -36% |
| Sedentary lifestyle | 69% | 21% | -69.60% |
| Obesity | 18.80% | 6.30% | -66.50% |
| Hypercholesterolemia | 13.80% | 6.1%, | -55.80% |
| (total cholesterol >6.2 mmol/L or 239.8 mg/dL) | |||
| Smoking | 43.30% | 33.60% | -22.40% |
| Diabetes mellitus. | 4.90% | 4.70% | -4.10% |
| (fasting blood sugar >7.8 mmol/L or 140.4 mg/dL) | |||
| Hypertension | 27.40% | 32.40% | 18.20% |
Table 1: Modifiable risk factor variation in Cuba across the 1990s, as documented in the “10 de Octubre” Study (Reproduced with permission from Morales-Salinas [10]).
Figure 1: Averages of total cholesterol (mmol/L) from the "10 de Octubre"10 and ASCOT-LLA11 studies. Blue bars, initial (1988) cholesterol levels; crimson bars, final (1994) cholesterol levels (Reproduced with permission from Morales-Salinas [10]).
Extending the period of observation of the Cuban cardiovascular risk factor landscape from 1980-2010, other investigators confirmed the findings associated with Cuban economic deprivation in the mid-1990s [12]. Specifically, there was a fall in prevalence of both type 2 diabetes (DM) and coronary heart disease (CHD). In the rebound period, from 1994-2010, the prevalence of obesity and overweight rose 19.4 percentage points, followed by a 116% increase in DM prevalence and 140% increase in DM incidence. Six years into the rebound, in the period 2002 to 2010, DM mortality increased by 49% accompanied by a rise in CHD deaths [12,13]. The association between forced hypocaloric diets, transition to plant-based fare, weight loss, greater physical activity, lower CVR, and subsequent reversal was striking. Although unproved, one putative explanation for the rise in blood pressure was the unmeasured yet obvious rise in psychosocial stress during the Special Period.
Layered Deleterious Effects beyond Traditional Risk Factors
In considering the effects of catastrophic environmental, social and economic change, at one level the prevalence of major traditional risk factors and subsequent effects upon outcomes is of concern, as described above. There is a linear relationship between number and intensity of risk factors and subsequent cardiovascular (CV) outcomes [14,15]. Tracking of common risk factors from youth to adulthood, which receives greatest attention in health systems focused upon individual risk, is a well-documented phenomenon [16-18]. Importantly, tracking of risk factors and their precursors applies to later adverse changes in pathological findings, biomarkers, other evidence of subclinical disease, and overt clinical manifestations of CHD [19-21].
Ascending vertically with age, from children to young adults and older, there are innumerable negative exposures the population may endure which result in negative physical and mental effects over time. Such accumulated insults, unmeasured but assuredly present, track into adulthood to impair future health. Thus, in the example given above during the Special Period in Cuba, one would expect a spectrum of subclinical negative exposures linked to traditional risk factors which remain largely unrecognized.
Expanding horizontally to include the greater components of SDH, there are also cumulative micoinsults as granularity increases, with some consequences more direct than others. These may occur from economic instability (poverty, stress, unemployment, lack of opportunity, food insecurity, housting instability), within the social and community context (sanitation, discrimination, incarceration, civic participation, and lack of social cohesion and support), within the sphere of education (high school graduation, higher education, access to job training, early childhood development, access to mass media and educational opportunities), health and care (access, health literacy, medications, screening, testing, procedures), and neighborhood and built environment (access to foods supporting healthy eating patterns, quality of housing, public safety, environmental conditions, access to transportation) [22].
The evidence base also includes examinations of relationships of SES to CV outcomes or intermediaries. For instance, childhood SES may predict metabolic syndrome, impaired fasting glucose, and DM up to 31 years later in adulthood [23]. Socioeconomic mobility, thought to be dependent upon elasticity of income between parent and grown child, but perhaps better correlated with person-level rank association, does have a relationship with ensuing ideal CV health, but the life course of both is highly modifiable [24]. The implications of the latter data are uncertain, and may also be somewhat unique to the U.S., where income mobility is low, but certainly need consideration.
In the adult population, there is ample evidence that SDH and deficiencies in health systems are negatively associated with cardiovascular outcomes and mortality [25]. For example, in one large study 6 psychosocial and socioeconomic factors were linked with a higher risk of CV death: unemployment, depression, unmarried status, poor contact with friends or relatives, and lack of material and all independent of each other. The health gap resulting from inequality at multiple levels is immense [26,27]. Unfortunately, wealth-related national inequality renders secondary prevention with aspirin, β blockers, angiotensin-converting enzyme inhibitors, and statins unavailable or unaffordable in many global populations [22]. As a result, low SES in low- and middle-income countries create impediments in accessing essential life-giving resources, which threatens attainment of planned goals to control CV disease and NCD globally [28,29]. When WHO member states joined in 2011 to forge the 25 × 25 initiative with the goal of a 25% reduction in premature NCD mortality by 2025, no provisions for SES improvements were made [28-30]. Making matters worse, the deficiency in access is frequently accompanied by lack of programs that promote adherence to those medications. Unless significant changes are made in leveling both equity and SES soon, World Health Organization (WHO) targets of 50% use of essential medicines by 2025 will not be reached [30,31].
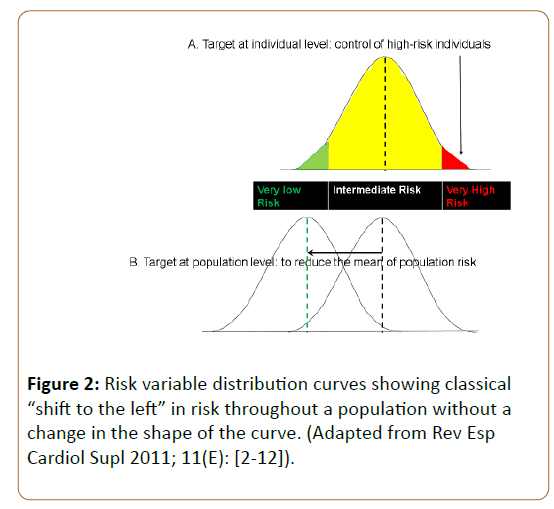
Population versus Individual Approaches-Revisiting Geoffrey Rose
The conceptual and theoretical foundation of population prevention is based on physician-epidemiologist Geoffrey Rose’s hypothesis that the most effective means of harnessing prevention is to shift the population distribution of risk factors to the left (Figure 2 and Table 2) [32]. Rose postulated that differences in the distribution of risk factors among populations have more influence upon cardiovascular mortality than the differences between individuals within the same population; further, that the subpopulation at low- to medium-risk gives rise to more cardiovascular deaths than those at high-risk, since the former is a vastly larger subgroup [7,32].
| Current Care | Future Care |
|---|---|
| Focused on the disease | Focused on the patient |
| Specialty and hospital care | Team effort based upon outpatient and community management |
| Focused on individual, high-risk patients | Focused upon on the needs of the population |
| Reactive, according to acute symptoms | Proactive, planned to forestall chronic manifestations |
| Focused on treatment | Focused on prevention |
| Single effects: block single enzymes, pathways, narrow targets | Multiple effects: synergistic, broad targets |
| Still authority-driven, but shared decision-making being incorporated | Patient education, empowerment, and self-care play inherently greater roles |
Table 2: Summary of general differences between current care, dominated by the cure of acute diseases with single causes, and future care, characterized by patient-centered, multipronged preventive approaches to achieve overall well-being.
Although some circumstances have changed and Dr. Rose’s views have been challenged, his population strategy remains valuable to improve overall population health and reduce social inequalities in the instant application [28]. The SDH interventions contemplated will shift the population distribution to the left without changing the shape of the curve, because they are not superficial, but fundamental and structural, addressing the context or circumstances within which behavior occurs, rather than upon individual agency [2,33,34]. Dr. Rose was also cognizant of using absolute, rather than relative risk measurements [35]. Since relative inequalities may be greater if a health factor is lower in prevalence, but absolute inequalities will remain low at both extremely high or low levels of prevalence, consistency in use of absolute values is emphasized [2,36].
The Chronic Care Model
The acute care model of managing disease developed and was matched to illnesses common in the past century, typically pretransition ailments such as infections and trauma [7]. Rapidly growing prevalence of chronic, degenerative “Diseases of civilization” have now extended globally to affect non-Western countries as “noncommunicable diseases” (NCDs). These diseases develop over longer latency periods, involve multiple contributory “causes”, require different diagnostic approaches, skill sets, multimechanistic therapies and monitoring, and frequently risk polypharmacy with attendant complications. One recurring fault in the health care system is multilevel fragmentation, in contrast to comprehensive, seamlessly integrated and sustainable care [37,38].
Chronic illness is defined by the need for continuing patient adjustments through interactions with a health care system. Most of the morbidity and mortality worldwide are now consequences of chronic diseases. In the U.S., as prevalence of multimoribities grows, chronic care accounts for an increasingly larger portion of health care resources. Initial contributions to the revisionist movement included the development of the chronic care model (CCM) in the 1990s, followed by growing interest and support of additional investigators and orgnizations [38-41]. The model envisioned uniting a systematic evidencedbased practice and guidelines for patient-centered chronic care to improve efficiency, outcomes, and cost between informed and motivated patients interacting with proactive, trained practice teams [37,38].
Focusing upon 6 interrelated components: Self-management support, delivery system redesign, clinical information systems, decision support, health care organization, and community resources, the model maintained that their improvement goals could be produced through system reform [37]. The literature reveals that successes were established using the CCM in some outcomes related to diabetes, hypertension, congestive heart failure, and asthma [38,39].
The WHO published its Innovative Care for Chronic Conditions to extend the CCM to NCDs [40]. The writers recognized a different type of care system was required, and addressed 8 essential elements for action in managing chronic care: Support a paradigm shift, manage the political environment, build integrated health care, align sectorial policies for health, use health care personnel more effectively, keep patient-centered care all-inclusive, involve the community, and assign prevention a high priority [40].
A final topic which has been the subject of much recent investigation, but yet remains in its infancy, is the extensive nature of how SDH and all lifestyle events influence health through epigenetic mechanisms. An understanding of epigenetic reprogramming may explain trends in cardio metabolic disease, but currently the extent and details are largely unknown. As big data analysis furthers precision medicine, perhaps the intersection of these domains will grow and offer useful therapeutic targets through which patient care may be improved.
Conclusion
The chronic care model is best suited for the management of the prevalent and costly diseases of civilization most nations face. The need for acute care will always persist, and hence the two approaches are not mutually exclusive. However, in order to improve control of cardiovascular risk, interventions with an exclusively clinical and individual scope are insufficient [7,26,34]. Continuing to conceptualize these choices as dichotomous may imperil an important opportunity which should not be overlooked. The corollary, CVR management should always take into account the balance between the clinical and public health approaches, was evident in the forging of the first International Consensus on mild hypertension with low to moderate CVR [2].
Achieving equity between and within countries to allow sufficient access to proven, basic therapies is an essential prerequisite for success in achieving international health goals. The great challenge of prioritizing and implementing cardiovascular preventive strategies will always is the optimal integration of all strengths and preventive opportunities available in society. Since risk factors now include SDH, it is even more apparent all options have not been employed, leaving immense potential unfulfilled. Motivation, collaboration, resolve, and persistence by all stakeholders are essential [41]. These assets transcend the boundaries of the health sector, and require the conscious and unconditional support of all facilities, particularly governmental agencies and non-governmental organizations [2,3,7,8,22,26,24,31,34,37].
References
- Marchal S, Vant Hof AWJ, Hollander M (2018) The new European guideline on cardiovascular disease prevention; How to make progress in general practice? Eur J Gen Pract 24: 57-59.
- Morales SA, Coca A, Olsen MH, Sánchez RA, Sebba-Barroso WK, et al. (2017) Clinical perspective on antihypertensive drug treatment in adults with grade 1 hypertension and low to moderate cardiovascular risk: An international expert consultation. Curr Probl Cardiol 42: 198–225.
- Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, et al. (2016) 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The sixth joint task force of the european society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European association for cardiovascular prevention & rehabilitation (EACPR). Eur Heart J 37: 2315-2381.
- Stewart J, Manmathan G, Wilkinson P (2017) Primary prevention of cardiovascular disease: A review of contemporary guidance and literature. JRSM Cardiovasc Dis 6: 129.
- Kones R (2011) Primary prevention of coronary heart disease: Integration of new data, evolving views, revised goals, and role of rosuvastatin in management: A comprehensive survey. Drug Des Dev Ther 5: 325-380.
- Kones R, Rumana U (2015) Current treatment of dyslipidaemia: A new paradigm for statin drug use and the need for additional therapies. Drugs 75: 1187-1199.
- Kones R, Rumana U (2017) Cardiometabolic diseases of civilization, history and maturation of an evolving global threat: An update and call for action. Ann Med 49: 260-274.
- Kones R, Rumana U (2018) Cultural primer for cardio metabolic health, health disparities, structural factors, community, and pathways to improvement. Postgrad Med 130: 200-221.
- Debs PG, De La NGR, Dueñas HA, González PJC (2001) Prevalence of coronary risk factors in "october 10", its evolution to 5 years. Rev Cubana Cardiol Cir Cardiovasc 15: 14-20.
- Morales SA (2013) Cuban economic crisis of the 90s and obesity: The "pictures" that left "october 10". Rev Fed Arg Cardiol 42:1-3.
- Sever PS, Dahlöf B, Poulter NR, Wedel H, Beevers M, et al. (2003) Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower than average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial - Lipid Lowering Arm (ASCOT-LLA): A multicentre randomised controled trial. Lancet 361: 1149-1158.
- Bilal MFU, Orduñez P, Benet M, Morejón A, Caballero B, et al. (2013) Population wide weight loss and regain in relation to diabetes burden and cardiovascular mortality in Cuba 1980-2010: Repeated cross sectional surveys and ecological comparison of secular trends. BMJ 346: 1515.
- www.theatlantic.com/health/archive/2013/04/how-cubans-health-improved-when-their-economy-collapsed/275080/
- Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, et al. (2012) Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA 307: 1273-1283.
- Kones R (2011) Is prevention a fantasy, or the future of medicine? A panoramic view of recent data, status, and direction in cardiovascular prevention. Ther Adv Cardiovasc Dis 5: 51-61.
- Kones R, Rumana U (2014) Prevention of cardiovascular disease: Updating the immensity of the challenge and the role of risk factors. Hospital Practice 42: 92-100.
- Chen W, Srinivasan SR, Ruan L, Mei H, Berenson GS, et al. (2011) Adult hypertension is associated with blood pressure variability in childhood in blacks and whites: The Bogalusa heart study. Am J Hypertens 24: 77-82.
- Kristensen PL, Wedderkopp N, Møller NC, Andersen LB, Bai CN, et al. (2006) Tracking and prevalence of cardiovascular disease risk factors across socio-economic classes: A longitudinal substudy of the European youth heart study. BMC Public Health 6: 20.
- Homma S, Troxclair DA, Zieske AW, Malcom GT, Strong JP, et al. (2011) Pathobiological determinants of atherosclerosis in youth research group (2011) histological changes and risk factor associations in type 2 atherosclerotic lesions (fatty streaks) in young adults. Atherosclerosis 219: 184-190
- Aatola H, Hutri KN, Juonala M, Laitinen TT, Pahkala K, et al. (2014) Prospective relationship of change in ideal cardiovascular health status and arterial stiffness: The cardiovascular risk in young finns study. J Am Heart Assoc 3: e000532.
- Hartiala O, Kajander S, Knuuti J, Ukkonen H, Saraste A, et al.(2016) Life-course risk factor levels and coronary artery calcification. The Cardiovascular Risk in Young Finns Study. Int J Cardiol 225:23-29.
- www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health
- Puolakka E, Pahkala K, Laitinen TT, Magnussen CG, Hutri-Kähönen N, et al. (2016) Childhood socioeconomic status in predicting metabolic syndrome and glucose abnormalities in adulthood: The cardiovascular risk in young finns study. Diabetes Care 39: 2311-2317.
- Pollock BD, Harville EW, Mills KT, Tang W, Chen W, et al. (2018) Cardiovascular risk and the american dream: Life course observations from the BHS (Bogalusa Heart Study). J Am Heart Assoc 7: e007693.
- Tillmann T, Pikhart H, Peasey A, Kubinova R, Pajak A, et al. (2017) Psychosocial and socioeconomic determinants of cardiovascular mortality in Eastern Europe: A multicentre prospective cohort study. PLoS Med 14: e1002459.
- www.bloomsbury.com/uk/the-health-gap-9781408857991
- Khatib R, McKee M, Shannon H, Chow C, Rangarajan S, et al. (2016) Availability and affordability of cardiovascular disease medicines and their effect on use in high-income, middle-income, and low-income countries: An analysis of the PURE study data. Lancet 387:61-69.
- www.un.org/sustainabledevelopment/sustainable-developmentgoals/
- apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf
- Stringhini S, Carmeli C, Jokela M, Avendaño M, Muennig P, et al (2017) Lifepath consortium. Socioeconomic status and the 25ÃÆâÃâââ¬ÃâÃâ ×ÃÆâÃâââ¬ÃâÃâ 25 risk factors as determinants of premature mortality: A multicohort study and meta-analysis of 1.7 million men and women. Lancet 389:1229-1237.
- Murphy A, Palafox B, O'Donnell O, Stuckler D, Perel P, et al. (2018) Inequalities in the use of secondary prevention of cardiovascular disease by socioeconomic status: Evidence from the pure observational study. Lancet Glob Health 6: e292–301.
- Rose G (1985) Sick individuals and sick populations. Int J Epidemiol 14: 32-38.
- McLaren L, McIntyre L, Kirkpatrick S (2010) Rose's population strategy of prevention need not increase social inequalities in health. Int J Epidemiol 39: 372-377.
- Morales Salinas A, Kones R (2018) Barriers to global action plan for the prevention and control of noncommunicable diseases: Proposal modifications to the voluntary targets. J Prev Med 3: 1.
- Rose G (1992) The strategy of preventive medicine. oxford: Oxford university press.
- Houweling TAJ, Kunst AE, Huisman M, Mackenbach JP (2007) Using relative and absolute measures for monitoring health inequalities: Experiences from cross-national analyses on maternal and child health. Int J Equity Health 6:15.
- Hall J (2015) Australian health care: The challenge of reform in a fragmented system. N Engl J Med 373: 493-497.
- O’Connor SJ (2014) Fragmentation is a prominent feature of the American healthcare landscape. J Healthc Manag 59:1–2.
- Wagner EH, Austin BT, Von Korff M (1966) Organizing care for patients with chronic illness. Milbank Q 74: 511-544.
- www.improvingchroniccare.org/downloads/who_innovative_care_for_chronic_conditions.pdf
- Morales Salinas A, Baranchuk A, Bayés de Luna A (2017) Ibero-American collaboration in medwave. concerning world heart day. Medwave 17: e6883.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences