Assessment as a Prognostic Marker by Meta-analysis of the Neutrophil/Lymphocyte Ratio in Acute Stroke
Fernando Fuertes-Guiro* and Elena Camiran-Blesa
Fernando Fuertes-Guiro1* and Elena Camiran-Blesa2
1Department of Medicine, Faculty of Medicine and Health Sciences, International University of Catalonia, Barcelona, Spain
2Faculty of Medicine and Health Sciences, University Hospitals Quiron Salud, Barcelona, Spain
- Corresponding Author:
- Fernando Fuertes-Guiro
Faculty of Medicine and Health Sciences
International University of Catalonia
General Hospital of Catalonia, Barcelona, Spain
Tel: +34 93 504 2000
E-mail: fernandofuer@gmail.com
Received date: November 06, 2019; Accepted date: January 20, 2020; Published date: January 27, 2020
Citation: Fuertes-Guiro F (2020) Assessment as a Prognostic Marker by Meta-Analysis of the Neutrophil/Lymphocyte Ratio in Acute Stroke. J Prev Med Vol. 5 Iss No. 1: 2.
Copyright:© 2020 Fuertes-Guiro F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Certain markers of inflammatory response are emerging in many studies as prognostic factors in pathological processes with an inflammatory basis, such as acute stroke. The objective of this paper is to analyze the capacity of the neutrophil/lymphocyte ratio to determine the prognostic value in this pathology by a meta-analysis and systematic review of the literature.
Methods: An exhaustive bibliographical review of articles that assessed the neutrophil-lymphocyte ratio was performed for the period 1995-2018, with an evaluation by meta-analysis with subgroups (ratio value, pathological subtype and country of origin).
Results: Fifteen studies (3,857 patients from 7 countries) were included in the study. Neutrophil/lymphocyte ratios ≥ 5 were significantly related to poor survival, regardless of pathologic subtype (prediction is stronger in the ischemic processes), and origin (oriental studies are more predictive).
Conclusion: In this meta-analysis, elevated levels of NLR obtained in the first 24 h are associated with a worse short-term prognosis in patients with stroke (ischemic and hemorrhagic). To corroborate these results will be necessary to carry out prospective studies with large cohorts of patients. The NLR is an index that is obtained from the routine analysis in the emergency room and its cost is economic, so it could be used routinely in the initial evaluation of the prognosis of the acute stroke.
Keywords
Inflammatory response; Acute stroke; Platelets; Immune system
Introduction
It is widely accepted that the systemic inflammatory response is related to cardiovascular diseases [1]. Many hematological parameters that are part of the inflammatory response, such as the amount of neutrophils, monocytes and platelets, as well as some inflammatory indices such as neutrophil/lymphocyte or platelet/lymphocyte ratio have been considered indicators that may have prognostic implications (morbidity and mortality) for peripheral vascular diseases [2].
The neutrophil/lymphocyte ratio [NLR], calculated from the ratio between neutrophils and total lymphocytes, has a clinical value derived from the information it provides on the state of the patient's inflammatory activity, and in patients with an acute stroke, the intensity of the inflammatory process in the vascular bed where the lesion is located [3].
In recent years, numerous studies have indicated the prognostic value of this index in a wide variety of pathological processes [4-8], especially vascular and tumoral, but also endocrine, nephrological and infectious pathologies. There have also been recent reports relating an increase in this index to a poor prognosis for the patient’s evolution in numerous peripheral vascular diseases, in addition to stroke: acute limb ischemia, venous thromboembolism, mesenteric ischemia, vasculitis, acute coronary syndrome, cardiac rhythm disorders, and coronary bypass surgery [9].
The predictive value of the NLR seems to be due to two reasons [10].
1. It is the index that is least influenced by various physiological conditions such as exercise and dehydration.
2. It is an index that represents two complementary immunological pathways: neutrophils, which are responsible for the nonspecific inflammatory response, and lymphocytes, which are a marker of physiological stress.
After heart disease, stroke is the second most common cause of death in the Western world and is the leading cause of disability, especially among the senile population. Many efforts have been made at all levels, both pre-hospital and in hospital and in primary care, for the prevention and early treatment of this highly prevalent pathology.
Like other peripheral vascular diseases, it has been shown that the inflammatory response in a stroke is involved in all pathophysiological processes [11].
If small amounts of mediators of inflammation are found in the brain under normal conditions, when stroke [ischemic and hemorrhagic] is verified there is a significant release of cytokines and the appearance of opsonization of cells of the immune system, which are responsible for further increasing the initially vascular brain injury. As a fundamental part of the immune system, neutrophils and lymphocytes play an important role in this inflammatory response.
Several studies relating the evolution and prognosis of cerebrovascular diseases with high values of the neutrophil/ lymphocyte index have recently been published. However the predictive value of this index needs more studies to be acceptable as valid.
We propose to design a meta-analysis of the published studies that relate the prognosis of stroke with NLR based on the following objectives:
1. Perform a systematic review to determine the prognostic value of NLR in acute stroke
2. Evaluate the impact of CNL on the various subpathologies of stroke
3. Evaluate the determination of a valid cut-off value of NLR as a predictor of survival
Methodology
Search strategy, inclusion and exclusion criteria and final selection of articles
The meta-analysis was designed following the PRISMA guidelines [12]. The search for articles covered the following electronic databases: the ISI web of knowledge, MEDLINE, EMBASE, the Cochrane Library, Google Scholar and Scopus.
Only RCT articles and controlled clinical trials published in English during the period between 1995 and 2018 were included in the study.
The search strategy used the following keywords and phrases: "NLR" or "neutrophil/lymphocyte ratio and "stroke" or "acute intracerebral hemorrhage" or "acute ischemic stroke" and "survival" or "prediction." The selection process was performed as follows:
1. All the titles and abstracts of the initially selected papers that were related to the objectives of the work were identified and read by two reviewers. Disagreements were resolved by consensus.
2. Once the abstracts were identified and read by consensus, the two authors selected those that met the following inclusion criteria:
a. Studies comparing survival in stroke patients with high NLR and low NLR, and indicating an NLR cut-off value
b. Availability of a hazard ratio [HR] and 95% confidence interval [CI] or a p value for overall survival; and
c. When the same author had published more than one paper, the most recent and the one with the highest quality were selected
3. The exclusion criteria were as follows:
a. Trials that were not RCT or were comparative
b. Studies repeated in different journals
c. Non-clinical studies (communications to congresses, review articles, letters to the editor, editorials) and clinical cases
d. Articles without availability of the full text
4. Once the final works had been selected, those without sufficient standardized data for inclusion in a meta-analysis study were discarded
Data collection and quality assessment
The Newcastle-Ottawa scale [NOS] [13] was used to assess study quality. This scale comprises three quality parameters (selection from 0 to 4 points, comparability from 0 to 2 points, evaluation of results from 0 to 3 points).
A score higher than 6 represents a high quality of the study methodology.
The data selected for each study were authorship, year of publication, country of origin, number of patients recruited for the study, clinical presentation of stroke [ischemic or hemorrhagic], cut-off points in the peripheral blood of the NLR and hazard ratios, and 95% associated CIs for overall survival. The RH was obtained from multivariate analysis, and failing that, from univariate analysis.
Written informed consent was not necessary because no patient data has been included in the manuscript.
Clinicopathological and prognostic definitions
According to the WHO [14], cerebrovascular disease is the rapid development of clinical signs of disturbances of brain or global function, with symptoms persisting for 24 hours or longer, or leading to death with no other obvious cause than vascular origin. While this includes sub arachnoid hemorrhage, it excludes transient ischemic attacks, subdural hematomas and ischemic myocardial with other etiologies [septic or neoplastic emboli].
Cerebrovascular disease can occur in two ways:
• A hemorrhagic form, which depending on the size and location may be an intracerebral hematoma [ICH], lobar hematoma or subarachnoid hemorrhage [SAH].
• An ischemic form, with etiologies as follows: arteriosclerosis, cardiac embolism, penetrating, cryptogenic and unusual arteries (prothrombotic states, dissections, arteritis and drugs) disease.
The cut-off point is the threshold value of INL from which a poor prognosis of survival in patients affected by stroke is objectively observed. Blood samples to obtain the CNL value must be obtained within the first 24 hours after the diagnosis of stroke. The period evaluated in the forecast was defined and stated in each selected article.
Statistical analysis
The data obtained from the selected papers were analyzed in meta-analysis using RevMan5.3 software. We used the logarithm of the risk ratio [HR] primarily with the 95% confidence interval (CI) [24]. The HR data and 95% CI were obtained directly from each selected article or were calculated from indirect data [24]. The meta-analysis of the data was performed using the random effects model and the fixed effects model.
First a statistical analysis of the heterogeneity was made applying the statistical test of Higgins and Thomson (I²) and the test of χ2; The results were classified as low (I²<25%), moderate (I²=25 to 75%) or high (I²>75%) consistency considering significant values when p<0.05.
Subsequently the publication bias was explored analyzing the funnel plots and from the tests of Egger and Begg; When p<0.05, was considered significantly biased. Subgroup analyzes were performed according to cutoff points for NLR, cerebrovascular disease type and region; A p-value<0.05 was considered statistically significant, unless otherwise specified.
Results
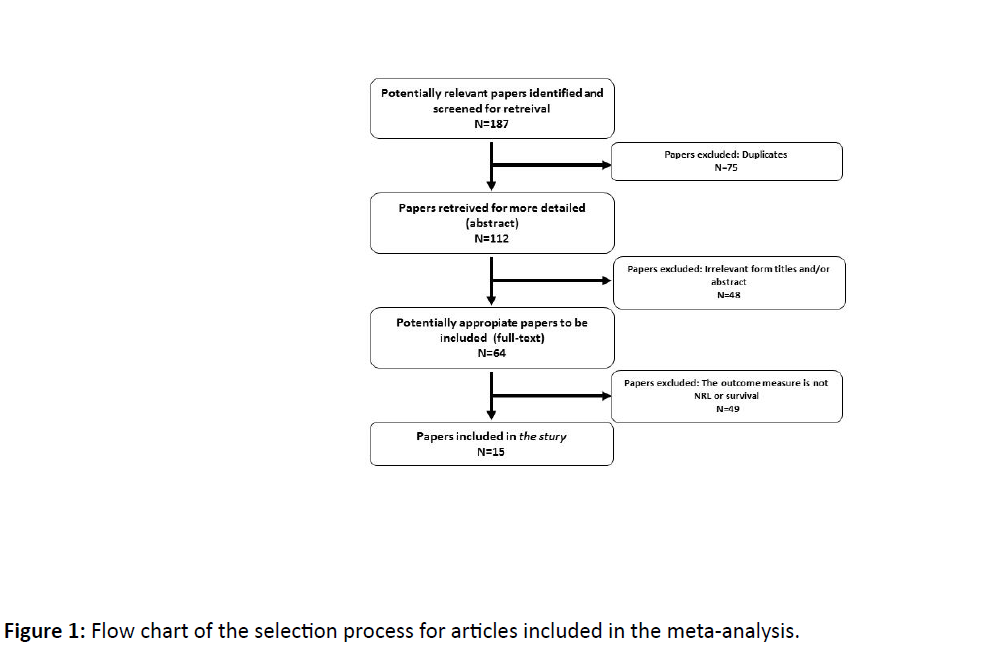
Fifteen studies [15-29] with a total of 3,857 patients were included in the meta-analysis (Figure 1).
Six studies were from Turkey, 4 from China, and 5 countries [Italy, Australia, the United States and Israel] produced 1 each. By pathology, 12 studies evaluated patients with ischemic stroke, and 5 with hemorrhagic stroke (Table 1).
| Reference year | Country | Design (period) | N(M-F) | Type of stroke | NLR cut offs | Prognostic value analysis | Survival outcomes |
|---|---|---|---|---|---|---|---|
| Brooks 2014 | USA | Retrospective | 116(53-63) | AIS | 5.9 | NLR | OS |
| Celikbilek 2013 | Turkey | 190(77-113) | AIS | 4.1 | NLR | OS | |
| Erdogan E 2013 | Turkey | 126(52-74) | AIS | NR | NLR | OS | |
| Farah R 2017 | Israel | 200(118-82) | AIS | NR | NLR | OS | |
| Gokhan 2013 | Turkey | 868(450-418) | AIS-AHS-TIA | NR | NLR | OS | |
| Lattanzi 2016 | Italy | 117(63-114) | AHS | 4.58 | NLR | OS | |
| Lok U 2016 | Turkey | 164(85-79) | AIS | NR | NLR | OS | |
| Luo P 2016 | China | 429(187-242) | AHS | 2.579 | NLR | OS | |
| Pagram 2016 | Australia | 142( NR ) | AIS | NR | NLR | OS | |
| Qun S 2017 | China | 143(80-63) | AIS | 2.99 | NLR | OS | |
| Sun Y 2016 | China | 352(234-118) | AHS | NR | NLR | OS | |
| Tokgoz 2013 | Turkey | 255(125-130) | AIS | NR | NLR | OS | |
| Tokgoz 2014 | Turkey | 151(81-70) | AIS | 4.81 | NLR | OS | |
| Wang 2015 | China | 224(141-83) | AHS | 7.35 | NLR | OS | |
| Xue J 2016 | China | 280(173-107) | AIS | 2.39 | NLR | OS |
Table 1: Characteristics of the studies included in the meta-analysis.
The study of the quality of the papers included in this systematic review obtained high scores on the Newcastle- Ottawa scale [NOS], indicating that the methodologies applied were adequate.
About eight of the studies calculated the cut-off value, with a mean + SD of (5.04 ± 0.90), a lowest cut-off of 2.39 and highest cut-off of 7.35. All studies evaluated survival.
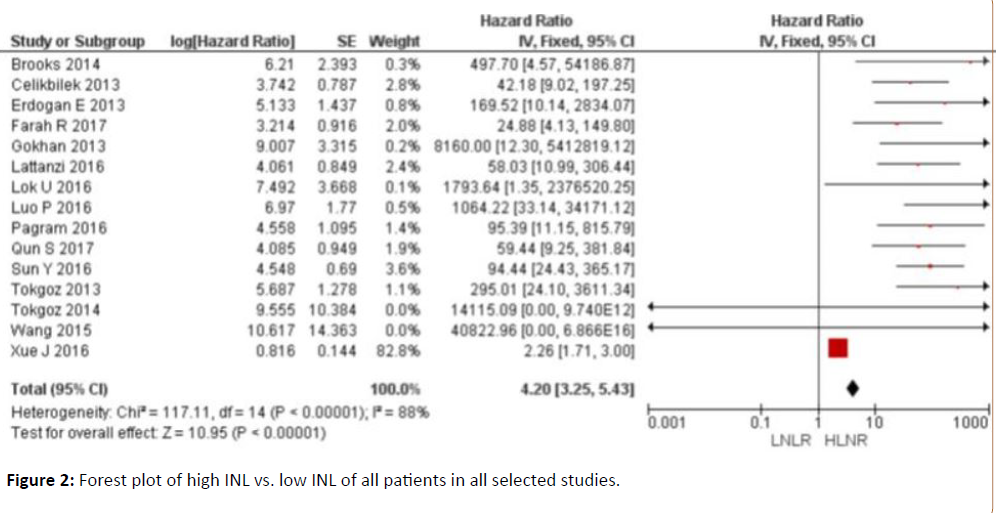
The total value of the hazard ratios, which was 4.2 (3.25-5.43) indicates that NLR could be used as a prognostic factor in the evaluation of stroke patients with an affected clinical status. The NLR values are inversely proportional to the favorable evolution of the patients. Of all the studies included in the study, Xue J [2016] has the highest proportional weight (82.8%) compared to the other studies included, with a hazard ratio of 2.26 (1.71-3) (Figure 2).
When the data selected by subgroups were analyzed by meta-analysis, the results obtained were as follows (Table 2 and Figures 3-6):
| Subgroup | N | HR (95% CI) P/RE FE | I2 | (%) | P | P for subgroup difference/RE FE | |||
|---|---|---|---|---|---|---|---|---|---|
| Cut-offs for NLR | 0.96 | 0.05 | |||||||
| <3 | 7 | 1.23 (1.19,1.28) | <0.00001 | 1.23 (1.19,1.28) | <0.00001 | 0% | 0.65 | ||
| 3-4 | 6 | 1.22(1.13,1.32) | <0.00001 | 1.22 (1.13,1.32) | <0.00001 | 6% | 0.38 | ||
| NLR>5 | 5 | 1.21 (1.03,1.42) | 0.02 | 1.13 (1.06,1.20) | 0.0003 | 80% | <0.00001 | ||
| Type of treatment | 0.07 | 0.07 | |||||||
| Chemotherapy | 5 | 1.20 (1.12,1.29) | <0.00001 | 1.10 (1.04,1.17) | 0.002 | 0% | 0.88 | ||
| surgery | 5 | 1.31 (1.23,1.41) | <0.00001 | 1.31 (1.23,1.41) | <0.00001 | 0% | 0.50 | ||
| Pathological type | 0.11 | 0.03 | |||||||
| NSCLC | 14 | 1.24 (1.20,1.28) | <0.00001 | 1.24 (1.20,1.28) | <0.00001 | 2% | 0.43 | ||
| SCLC | 4 | 1.15 (1.06,1.25) | 0.001 | 1.14 (1.07,1.22) | <0.0001 | 35% | 0.20 | ||
| Region | 0.53 | 0.50 | |||||||
| Eastern countries | 15 | 1.22 (1.17,1.27) | <0.00001 | 1.21 (1.18,1.25) | <0.00001 | 23% | 0.20 | ||
| Westren countries | 3 | 1.28 (1.11,1.48) | 0.0006 | 1.25 (1.15,1.37) | <0.00001 | 49% | 0.14 | ||
FE: Fixed-Effect Model; HR: Hazard Ratio; RE: Random-Effect Model; NSCLC: Non-Small Cell Lung Cancer; N: Number; NLR: Neutrophil-To-Lymphocyte Ratio; SCLC: Small Cell Lung Cancer
Table 2: Sensitivity analysis by sub-groups.
1. NLR values:
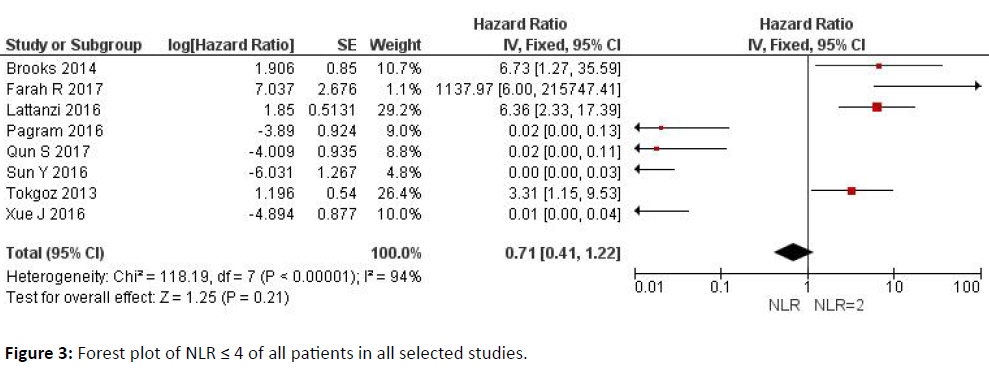
With values of 2, a total value of hazard ratios of 0.45 (0.27-0.76) was observed, while for values of 3-4 the total value of hazard ratios was 0.71 (0.41-1.22), indicative of a better prognosis (low heterogeneity).
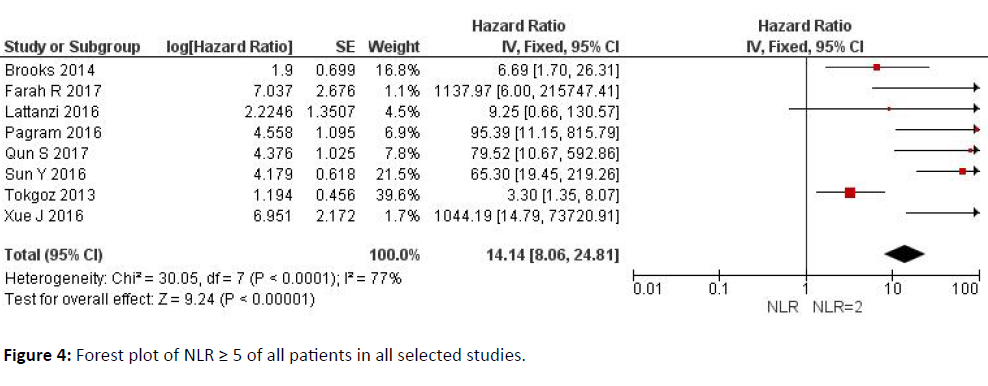
NLR values above 5 indicate an evolution of the clinical course with a poor prognosis, with hazard ratios of 14.14 (8.06-24.81). These values are statistically significant in the analysis of the subgroups.
2. Clinical form of stroke:
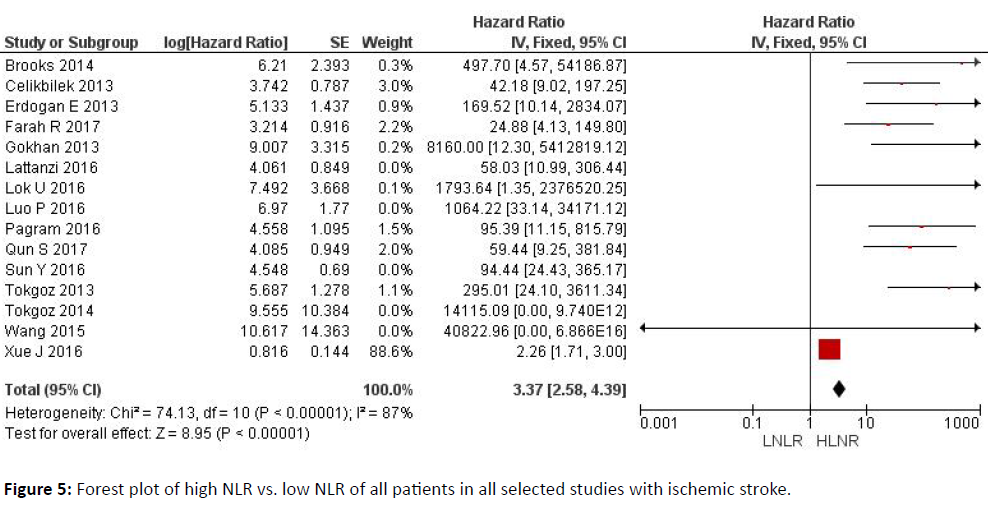
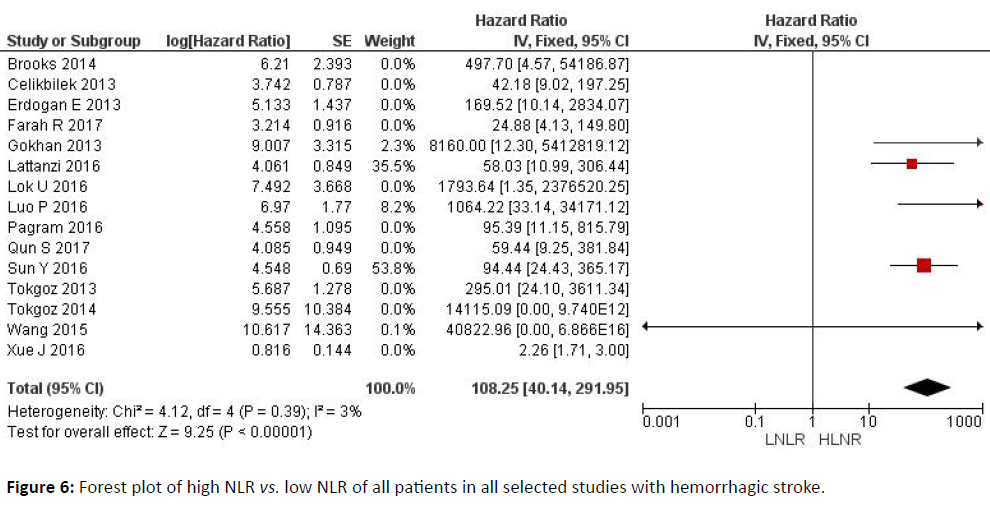
With both clinical forms of stroke [ischemic and hemorrhagic], a high NLR might be indicative of a worse prognosis, with greater predictive strength in the ischemic variant (total hazard ratio value of 3.37 (2.58-4.39) (p<0.00001)) than in the hemorrhagic form (108.25 (40.14-291.95)).
3. By country:
Both Western and Eastern countries show a relationship between the predictive value of stroke and high NLR values.
However, the predictive value is reinforced in Eastern countries: the total value of hazard ratios is 93.70 (36.99-237.34) (p<0.00001).
Figure 3 explains the data analyzed of the Neutrophil- Lymphocyte Ratio (NLR) of the studies with ≤ 4 of the patients in all the conducted studies.
Figure 4 explains the data with a forest plot for Neutrophil-Lymphocyte Ratio (NLR) ≥ 5 of all patients in all selected studies.
Figure 5 explains the forest plot of high NLR vs. low NLR of all patients in all selected studies with ischemic stroke.
Figure 6 explains the forest plot of high NLR vs. low NLR of all patients in all selected studies with hemorrhagic stroke. All the data used have been thoroughly scrutinized and final conclusions have been drawn respectively.
Finally, in the analysis of publication bias, in both the Begg test where we obtained a value of Z=1.0445(p=0.2963>0.05) and in the Egger test where we obtained a value of t=-3.7580(p=0.1656>0.05), there was no apparent publication bias.
Discussion
In vascular pathophysiology, it is widely known that an inflammatory response occurs after a vascular [ischemic or hemorrhagic] process, which can in turn lead to an aggravation of the tissue injury. As in any other organ, in the brain, after an acute stroke, the reactive inflammatory process has two distinct periods: first, after 6-12 hours, when a PNL infiltrate releases large amounts of inflammatory mediators which are also able to further injure brain tissue; and a second period after 3-6 days, when large amounts of lymphocytes are known to play a prominent role in the neutralization of the leukocyte cytokines in the injured area, promoting the repair of the destroyed tissue [30].
Based on these findings, many studies have linked the variations of these two cell populations in the prognosis of severity and extent of brain injury during stroke [31,32]. More recently, and in the light of the two roles that PNL and lymphocytes represent, numerous articles based on the predictive effect of the NLR in cardiovascular pathologies have been published [33]. The many articles that point to a positive predictive effect of low numbers of this cellular quotient nevertheless require meta-analytical studies to make these results consistent with an acceptable scientific rigor if they are to be taken into account in daily clinical practice. In this paper, the prognostic value of NLR in stroke patients has been evaluated through a meta-analysis, based on a systematic review of the literature. The results show that high levels of CNL are associated with a poorer prognosis for patients, an increase in leukocyte activity (cell membrane damage by proteolytic enzymes, arachidonic acid, elastase, and oxygenfree radicals), and reduced lymphocyte activity (mechanisms regulating the immune response) could be responsible for a poorer clinical evolution. These cellular and micro vascular findings have already been reported [34-40].
In order to select patients more homogeneously in the meta-analysis, the papers selected had to meet inclusion and exclusion criteria. The former included a clinical-radiological diagnosis, and the blood samples being obtained within 24 hours of the beginning of the pathological process. The exclusion criteria included patients with traumatic brain injury, neoplasms, active infectious process, and previous treatment with immunomodulators, haemopathies, inflammatory diseases, renal or hepatic pathology, acute metabolic disease and intoxication. These criteria are necessary to be able to better evaluate the cut-off value to be taken into account as a predictive value [41].
To further investigate the predictive factor of NLR, the data obtained from the selected studies were divided into three variables.
These variables were: value of NL ratio, pathophysiological subtype of stroke (ischemic or hemorrhagic), and country of origin of patients (Eastern and Western). The subgroup sensitivity study indicated that a cut-off NLR below 4 provided a good prognosis for survival in all patients included in the meta-analysis, and a value above 5 provided a poor prognosis, which all suggested that the prognosis is worse when the inflammatory process in the injured area is intense. These results corroborate previous findings at the cellular level. Meanwhile, a high NLR index is predictive of a worse prognosis for the two clinical forms considered for stroke, although the prediction is stronger in the ischemic processes, although the NLR values are lower in the latter, possibly due to the hemorrhagic phenomenon developing a more extensive inflammatory process [19]. The origin of the patients makes no difference in the predictive value of the NLR, and although the Eastern studies have more statistical strength, this cannot in principle be associated to any specific justification.
Conclusion
Based on the results of this meta-analysis, the prognosis of NLR survival in a patient with stroke could have some limitations. First, it is limited in time, since published articles examine periods shorter than three months after the stroke diagnosis. Having a more extensive follow up in the future will ensure the predictive value of the NLR sometime after the event. Second, although the studies were selected based on the inclusion and exclusion criteria and although the heterogeneity observed in the meta-analysis is low and the Newcastle-Ottawa score is high, there is some heterogeneity in the specific characteristics of the researchers in terms of their approach to their research. This heterogeneity is apparent in the relationship between NLR and survival, and is due to the non-uniform cut-off value of NLR [Range: 2.39-7.35]. On the other hand, there is clinical heterogeneity because the studies differ in the treatment applied. Third, because only English language publications were included, language bias should also be considered in the selection of the papers selected.
What is the practical application of the NLR value? This meta-analysis reveals that high NLR values, and particularly values higher than 5, are associated with poor prognosis of short-term survival. However, as it is a non-uniform cutoff value - according to the various papers published and included in this study, it would be difficult to apply for clinical use. These results therefore warrant confirmation in cohort studies of large samples with a final NLR cutoff value. The NLR is a parameter that can be calculated from routine data used in emergencies and is not expensive, and its application could be systematic. In conclusion, in this meta-analysis, elevated levels of NLR obtained in the first 24 hours are associated with a worse short-term prognosis in patients with stroke (ischemic and hemorrhagic). It will be necessary to carry out prospective studies with large cohorts of patients to corroborate these results. The NLR is an index that is obtained from routine analysis in the emergency room, and its cost is economical, so it could be used routinely in the initial evaluation of the prognosis of acute strokes.
References
- Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, et al. (2003) Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from Centers for Disease Control and Prevention and the American Heart Association. Circulation 107: 499-511.
- Fowkes FG, Rudan D, Rudan I, Aboyans V, Denenberg JO, et al. (2013) Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet 382: 1329-1340.
- Ünlü M, Arslan Z (2015) The relation between neutrophil-lymphocyte ratio and endothelial dysfunction. Angiology 66: 694.
- Mei Z, Shi L, Wang B, Yang J, Xiao Z, et al. (2017) Prognostic role of pretreatment blood neutrophil-to-lymphocyte ratio in advanced cancer survivors: A systematic review and meta-analysis of 66 cohort studies. Cancer Treat Rev 58: 1-13.
- Bhat TM, Afari ME, Garcia LA (2016) Neutrophil lymphocyte ratio in peripheral vascular disease: a review. Expert Rev Cardiovasc Ther 14: 871-875.
- Paquissi FC (2016) The role of inflammation in cardiovascular diseases: the predictive value of neutrophil-lymphocite ratio as a marker in peripheral arterial disease. Therapeutics Clin Risk Manag 12: 851-860.
- Yang HB, Xing M, Ma LN, Feng LX, Yu Z (2016) Prognostic significance of neutrophil-lymphocyteratio/platelet-lymphocyteration in lung cancers: a meta-analysis. Oncoarget 22: 7676978.
- Proctor MJ, McMillan DC, Morrison DS, Fletcher CD, Horgan PG, et al. (2012) A derived neutrophil to lymphocyte ratio predicts survival in patients with cancer. Br J Cancer 107: 695-699.
- Küçük E, Kocayiğit İ, Günel C, Düzenli H (2016) Neutrophil-to-lymphocyte ratio in occlusive vascular diseases: the literature review of the past 10 years. World J Emerg Med 7: 165-172.
- Oh SH, Kim OJ, Shin DA, Song J, Yoo H, et al. (2012) Alteration of immunologic responses on peripheral blood in the acute phase of ischemic stroke: blood genomic profiling study. J Neuroimmunol 249: 60-65.
- Chamorro A and Hallenbeck J (2006) The harms and benefits of inflammatory and immune responses in vascular disease. Stroke 37: 291-293.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151: W65-W94.
- http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- Brooks SD, Spears C, Cummings C, VanGilder RL, Stinehart KR, et al. (2014) Admission neutrophil-lymphocite ratio predicts 90 day outcome after endovascular stroke therapya. J Neurointerv Surg 6: 578-583.
- Celikbilek A, Ismailogullari S, Zarazsiz G (2014) Neutrophil to lymphocite ratio predicts poor prognosis in ischemic cerebrovascular disease. J Clin Lab Anal 28: 27-31.
- Ertas G, Sönmez O, Turfan M, Erdogan E, Tasal A, et al. (2012) Neutrophil/lymphocite ratio is associated with thromoboembolic stroke in patients with non-valvular atrial fibrillation. J Neurol Sci 324: 49-52.
- Farah R, Samra N (2017) Mean platelets volume and neutrophil to lymphocite ratio as predictors of stroke. J Clin Lab Anal 32: e22189.
- Gökan S, Ozhasenekler A, Mansur Durgun H, Akil E, Ustündag M, et al. (2013) Neutrophil lymphocite ratios in stroke subtypes and transient ischemic attack. Eur Rev Med Pharmacol Sci 17: 653-657.
- Lattanzi S, Cagnetti C, Provinciali L, Silvestrini M (2016) Neutrophil to lymphocite ratio predicts the outcome of acute intracerebral hemorrhage. Stroke 47: 1654-1657.
- Lök U, Gülaçti U (2016) The predictive effect of the Neutrophil to lymphocite ratio [NLR] on the mortality of acute ischemic stroke and its subtypes: a retrospective cross-sectional study. Eurasian J Emerg Med 15: 69-72.
- Luo P, Li R, Yu A, Xu T, Yue S, et al. (2017) The relationship between neutrophil to lymphocite ratio and intracerebral hemorrhage in type 2 diabetes mellitus. J Stroke Cerebrovasc Dis 26: 930-937.
- Pagram H, Bivard A, Lincz L, Levi C (2016) Peripheral Immune cell counts and advanced imaging as biomarkers of stroke outcome. Cerebrovasc Dis Extra 6: 120-128.
- Qun S, Tang Y, Sun J, Liu Z, Wu J, et al. (2017) Neutrophil to lymphocite ratio predicts 3-month outcome of acute ischemic stroke. Neurotox Res 31: 444-452.
- Sun Y, You S, Zhong C, Huang Z, Hu L, et al. (2017) Neutrophil to lymphocite ratio and the hematoma volumen and stroke severity in acute intracerebral hemorrhage patients. Am J Emerg Med 35: 429-433.
- Tokgoz S, Keskin S, Kayrak M, Seyithanoglu A, Ogmegul A (2014) Is neutrophil to lymphocite ratio predict to short-term mortality in acute cerebral infarct independently from infarct volumen? J Stroke and Cerebrovasc Dis 23: 2163-2168.
- Tokgoz, Kayrak M, Akpinar Z, Seyithanoglu A, Güney F, et al. (2013) Neutrophil to lymphocite ratio as a predictor of stroke. J Stroke Cerebrovasc Dis 22: 1169-1174.
- Wang F, Hu S, Ding Y, Ju X, Wang L, et al. (2016) Neutrophil to lymphocite ratio and 30-day mortality in patients with acute intracerebral hemorrhage. J Stroke Cerebrovasc Dis 25: 182-187.
- Xue J, Huang W, Chen X, Li Q, Cai Z, et al. (2017) Neutrophil to lymphocite ratio is a prognostic marker in acute ischemic stroke. J Stroke Cerebrovasc Dis 26: 650-657.
- Xi G, Keep RF, Hoff JT (2006) Mechanisms of brain injury after intracerebral haemorrhage. Lancet Neurol 5: 53-63.
- Vidale S, Consoli A, Arnaboldi M, Consoli D (2017) Post-ischemic inflammation in acute stroke. J Clin Neurol 13: 1-9.
- Bonaventura A, Liberale L, Vecchié A, Casula M, Carbone F, et al. (2016) Update on inflammatory biomarkers and treatments in ischemic stroke. Int J Mol Sci 17: 12.
- Afari ME and Bhat T (2016) Neutrophil to lymphocyte ratio [NLR] and cardiovascular diseases: an update. Expert Rev Cardiovasc Ther 14: 573-577.
- Galea J and Brough D (2013) The role of inflammation and interleukin-1 in acute cerebrovascular disease. J Inflamm Res 6: 121-128.
- Chalela JA, Merino JG, Warach S (2004) Update on stroke. Curr Opin Neurol 17: 447-451.
- Demuth HU, Dijkhuizen RM, Farr TD, Gelderblom M, Horsburgh K, et al. (2017) Recent progress in translational research on neurovascular and neurodegenerative disorders. ISN&N meeting contributors. Restor Neurol Neurosci 35: 87-103.
- An C, Shi Y, Li P, Hu X, Gan Y, et al. (2014) Molecular dialogs between the ischemic brain and the peripheral immune system: dualistic roles in injury and repair. Prog Neurobiol 115: 6-24.
- Del Zoppo GJ (2009) Relationship of neurovascular elements to neuron injury during ischemia. Cerebrovasc Dis 27 Suppl 1: 65-76.
- Nagy Z, Nardai S (2017) Cerebral ischemia/reperfusion injury: From bench space to bedside. Brain Res Bull 134: 30-37.
- Camós S, Mallolas J (2010) Experimental models for assaying micro vascular endothelial cell pathophysiology in stroke. Molecules 15: 9104-9134.
- Erturk M, Cakmak HA, Surgit O, Celik O, Aksu HU, et al. (2014) Predictive value of elevated neutrophil to lymphocyte ratio for long-term cardiovascular mortality in peripheral arterial occlusive disease. J Cardiol 64: 371-376.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences