Assessment of Injection Pattern of Use and Safety in Primary Health Care Facilities of Idku City, EL Beherah Governorate
Aida Mohey Mohamed*, Heba Mahmoud Taha El weshahi and Reham Abd El Rahman El Halawany
Department of Medicine, Alexandria University, Alexandria, Egypt
- *Corresponding Author:
- Aida Mohey Mohamed
Department of Medicine, Alexandria University, Alexandria, Egypt
Tel: 20 31227929039
E-mail: aida_mohey@yahoo.com
Received date: December 23, 2019, Manuscript No. IPJPM-19-3114; Editor assigned: December 26, 2019, PreQC No. IPJPM-19-3114 (PQ); Reviewed date: January 09, 2020, QC No. IPJPM-19-3114; Revised date: June 28, 2022, QI No. IPJPM-19-3114 (QI); Manuscript No. IPJPM-19-3114 (R); Published date: July 26, 2022, DOI: 10.36648/2572-5483.7.5.143.
Citation: Mohamed AM, El weshahi HMT, Hala wan y RAR (2022) Assessment of Injection Pattern of Use and Safety in Primary Health Care Facilities of Idku City, EL Beherah Governorate. J Prev Med Vol: 7 No: 5.
Abstract
Background: Unsafe injection practices and injection overuse are widespread in developing countries harming the patient and inviting risks to the health care workers. In Idku city, there is a dearth of documented data about injection practices in primary health care facilities. The aim of the present study was to assess pattern of injection use and to determine whether the studied facilities fulfill the conditions for safe injections practices and safe disposal.
Methods: A cross sectional study was conducted from August to December 2018 with injection prescribers and providers working at 12 Primary Health Care facilities (PHC) as well as injection recipients attending the facilities within Idku city, Egypt. Almost 720 prescriptions were reviewed, 46 locations for injections and 152 injection events were observed. A transfer-sheet was used to extract data from the prescriptions. A structured observational checklist was used for observing injection practice and interview formats were used for interviewing the study participants. Facility-based unsafe injection indicators were determined.
Results: Injection use rate was 50.0% (95% CI: 42.8-61.9). The prevalence of polypharmacy was 13.2%. Injections administered for curative purpose constituted 90.0% and 49.7% of these were prescribed for trace health conditions. Analgesics and antibiotics were most common prescribed injections. Almost 29.9% of patients prefer injections over non-injection medications. Policies/ guidelines and equipment for safe injections and disposal were sufficient in most of the facilities. Universal use of single use syringes and needles were observed. Deficiencies and unsatisfactory practices noted were that safety boxes are kept far from injection site, used injection equipment were seen outside the safety boxes or in an open containers, no hand washing or hand rub with alcohol, no sterilization of patient’s skin before injection, and non-using new needles for reconstitution. Around two-fifths of workers (42.1%) had suffered at least one Needle Stick Injury (NSI) in the last 6 months. Two-handed recapping and manual removal of needles were the common practices for NSIs. Post exposure prophylaxis was deficient in most of the facilities. Around 85.5% of the injection providers were vaccinated by 3 doses against hepatitis B.
Conclusion: Injections use in PHC facilities in Idku is high. The deficiencies noted in the practice and waste disposal must be addressed. Interventions for reduction of injection overuse and unsafe practices should be carefully implemented. Strategies should involve the three divers of unsafe injections; the prescribers, the injection providers, and the general population. The physicians should consider prescribing fewer unnecessary injections. The injection providers should be constantly trained and being supervised. The general population must become more aware of the consequences of unnecessary and unsafe injections.
Keywords
Primary health care; Injection use; Injection safety practices; Needle stick injury; Egypt
Introduction
Unsafe injection practices are common all over the world. According to the annual number of safe and unsafe injections, by WHO region, DHS surveys conducted in 2011-2015, it was found that the Eastern Mediterranean Region had the highest number of unsafe injections (0.376 per person per year) [1]. Because of the overuse of injections in numerous countries, unsafe injections cause a considerable extent of diseases with blood borne pathogens [2]. At risk of infection are injection recipients and service providers through contaminated needles and syringes and the community at large through exposure to contaminated sharps waste. A mathematical model has been used to estimate the burden of disease from unsafe injections in different locales. As indicated by gauges utilizing this model, unsafe injections represented 32% of hepatitis B virus infection, 40% of hepatitis C virus infection, 28% of liver cancer, 24% of cirrhosis and 5% of HIV infections in the year 2000 [3]. Overall, around 500 000 deaths every year are owing to contaminated injections in medical service settings worldwide [4].
Health Care Workers (HCWs) are exposed to Needle Stick Injuries (NSI) from unsafe practices. It is revealed that the most well-known clinical activity to cause NSIs was blood withdrawal, followed by suturing and vaccinations [5]. Health care workers acquire about 2 million Needle Stick Injuries (NSIs) every year as needle stick injuries present the single most prominent occupational hazard to medical personnel [6].
An injection is said to be safe if does not harm the recipient, does not expose the provider to any avoidable risk and does not bring about any waste that is hazardous for others [7]. Tool CRevised is structured by WHO to assess the safety of the most common procedures that puncture the skin within health services, including injections of different types, phlebotomy, lancet procedures, and common IV procedures such as infusions. The tool proposes a standardized methodology including concepts, study designs, sampling procedures, data collection methods and formats, and a plan for analyzing and reporting country safety assessments [8].
The 2015 WHO injection safety guidelines recommend utilization of safety-engineered injection devices such as Reuse Prevention (RUP) syringes for most therapeutic injections. It additionally recommends Sharps Injury Prevention (SIP) syringes. Auto Disable syringes (AD) are as of now being used in the immunization services globally. Their introduction along with matching supply of safety boxes, training and adequate supervision addressed the problem of reuse of injections in the EPI program. Reuse prevention and needle-stick injury protection syringes, especially in curative services, are the focal point of WHO recommendations, along with provision of sharps waste management equipment [9].
Injections have consistently been in popular demand for minor ailments at primary care facilities, in public and private settings. However, since not many years, Egypt has recognized that injection safety is an urgent priority that needs urgent consideration [10]. As part of a comprehensive strategy to prevent blood-borne pathogen transmission in Egypt, the Ministry of Health and Population (MoHP) has implemented a national program to promote infection control, safe transfusion practices, and safe injection practices. In injection safety project in Egypt, a review of available literature from 2000 to 2015 was carried out, which revealed that reuse of needles and syringes was between 20%-23%, while the number of injections per person per year was estimated to be 6.8. Unsafe disposal, after bending the needle, occurred following 23% of injections. In Egypt, injections are the favored mode of treatment by both patients and prescribers [11].
A national assessment on injection safety in 2016 was completed in eight governorates of Egypt covering health care facilities in the public and private sector, as well as informal providers within the community. A significant advancement and made progress in various areas have been come out. Ministry of Health and Population (MoHP) and the WHO country office are building up a national policy on injection safety which included country-wide utilization of RUP (re-use prevention) syringes for injections. In addition, Egypt conducted an economic modeling study on the effect of decreasing unnecessary and unsafe injections develop a communication strategy and provide standardized training to health workers on injection safety [12].
In Idku city of El Beherah governorate, there is an absence of documented data and studies on injection pattern of use and practices in primary health care system. Accordingly, this study was conducted to assist national authorities in assessing, and evaluating the national policy, plans and strategies for injection safety. The present study was carried out to determine injection pattern of use at the PHC facilities in Idku city, assess injection safety practices and safe disposal among PHC workers, and investigate the availability of equipment for safe injection practices and the safe disposal of the waste produced after injection in the PHC facilities.
Materials and Methods
A descriptive, facility-based cross sectional observational study was carried out from August to December 2018 in all primary health care facilities (centers and units) n=12 in Idku city. At each facility, all activities dealing with injection were included. These were injections provided in immunization room, emergency room, dental clinic, and family planning clinic.
The target population were all primary Health Care Workers (HCWs) in-charge working for at least six months at the selected primary health care facilities (n=207,83 physicians and 124 nurses, MoHP statistics 2017) as well as all injection recipients attending the facilities.
Units of observation
• Prescriptions reviews of the participant physicians, and pharmacists.
• Primary health care workers (physicians, dentists and nurses).
• Clients with respective dispensing encounters at the selected facility.
• Equipment and facilities for safe injection and disposal of the waste produced after injection in the PHC facilities.
Sample size calculation of prescriptions
For sample size calculation, we assumed an alpha error of 0.05, precision of 5%, a design effect of 2 and considered prevalence of injection use as unknown. Considering these assumptions and including 10% of missing or incomplete data and the need to adjust for possible confounders, it was determined that a sample size of 708 were required for the study. To round up and to cover further short-fall, a total sample of 720 prescriptions was considered. Inclusion: Encounters that took place during the period from August to December 2017 were included. Referral or vaccinations were excluded.
Injection pattern of use
For the purpose of the study, an injection was defined as “A skin-piercing event performed with a syringe and/or needle with the purpose of introducing a curative substance or vaccine into a patient by various routes”. Therefore, injections carried out for phlebotomy, blood transfusion and other purposes were excluded from the study. Information was collected through prescription reviewing, direct interviewing and observation in the 12 PHC facilities in Idku city. From each primary health care facility, 40 medical encounters from facility registers of the previous day were randomly selected by systematic sampling. Additionally, 20 encounters were reviewed prospectively using patient/client exit-interviews or at the pharmacy to collect information on injections prescribed in a medical encounter on the day of the interview as well as inquiry about patient preference of injections and reasons of contribution to injection overuse (n=240). Encounters were spread at regular intervals throughout the study period to minimize the bias due to seasonal variations or interruptions of the drug supply cycle.
Injection safety
A pre-designed, pilot-tested, semi-structured data collection interview format and observational checklist is adopted and modified from WHO guide line of revised injection safety assessment tool (Tool C-Revised of the WHO) was used as tool of the study [8].
The survey tool is divided into two parts. Part one collected the demographic data of respondents including age, qualification, gender, years of experience in PHC, their knowledge about the diseases transmitted by unsafe injection practices. Part two collected data pertaining to:
• Including vaccination, intramuscular injections, family planning injections, and dental injections (local anesthetic). The investigator observed a total of 152 injection events being administered by the injection providers. During each visit injection safety practices were observed in terms of injection preparation, administration of injection to the patients and disposal of syringe/medical waste in order to give a clear understanding of whether the health providers followed standard guidelines. The providers are aware of the observation which may have led them to modify their practices or responses (Hawthorn effect). To minimize the Hawthorn effect, the checklist used for the observation was not being shown to the providers.
• A total of 46 injection locations were observed in the selected PHC facilities in order to systematically assess the availability of injection safety equipment and supplies at the facility.
• This interview was conducted to collect data about using disposable needles, exposure to needle-sticks injury in the last 6 months, having a guideline for Post Exposure Prophylaxis (PEP), post-exposure counseling and prophylactic medications, training courses about injection safety in the last 2 years, and data about receiving hepatitis B vaccine.
• (immediate supervisor of injection provider) to collect data about availability of the policies and guidelines of injections, the rate of work in every clinic, stock availability of both disposable equipment and puncture-resistant sharp containers, and information about designated staff for handling waste.
Data collection
The selected PHC facilities were visited during office working hours (2 shifts). The observation checklist was completed by observing the injection events and health care waste management practices in the facility. Interviews with all the injection providers present at the time of the visit were conducted at the PHC facilities by the investigator herself using the interview formats. This was carried out during working hours, particularly in the afternoon when there are likely to be fewer patients (less workload). This interview was conducted to complete the interview formats.
Ethical issues
Informed written consent was sought from each study subject before interview and observation. Respondents’ identities are kept confidential to protect their anonymity, and they were ensured that the information they give are not be used for any purpose other than scientific research. The research was approved by the Research Ethics Committee of Faculty of Medicine, Alexandria University. All injection providers were informed that participation is completely voluntary and that they were free to withdraw at any time during the study without needing to provide reason. Prior official permission was obtained from respective PHC facility directors to observe the health care facilities, their waste disposal method, and injection events at their health care facilities. Briefing was done to the respective authority for purpose of the study.
Data management
The data generated from the study were manually checked for possible errors and inconsistencies before data entry using SPSS software package version 22. Means and Standard Deviation (SD) or median and Interquartile Range (IQR) was computed for continuous variables and proportions for categorical variables.
Results
Injection pattern of use at PHC facilities in Idku city
The average number of drugs prescribed per encounter was 2. 9 (minimum 1 and maximum 6). The prevalence of polypharmacy (defined as the use of five or more medicines) was 13.2%. Out of 1894 medication prescribed per encounters, 396 were prescribed injections (20.9%). Nearly half of prescriptions (49.7%, n=179) that contained injectable drugs (n=360), injections were used in certain trace health conditions (Tracer conditions were defined as common health problems for which injections appear to be used often while they are not medically justified). The most common injections prescribed for tracer conditions were analgesics (43.0%) and antibiotics (35.8%) (Table 1).
| Prescribing indicator | No. (n = 720) | % |
|---|---|---|
| Average number of drugs prescribed per encounter | ||
| (Man ± SD) | 2.9 ± 1.3 | |
| Minimum-maximum | 1-6 | |
| Percent of encounters had prescribed drug or more | ||
| One drug | 170 | 23.6 |
| Two drugs | 211 | 29.3 |
| Three drugs | 149 | 20.7 |
| Four drugs | 95 | 13.2 |
| Five drugs or more | 95 | 13.2 |
| The number of injections per prescription | ||
| None | 360 | 50.0 |
| One injection | 324 | 45.0 |
| Two injections | 36 | 5.0 |
| Percent of prescribed injections to total medication prescribed | 396/1894 | 20.9 |
| Injection used in certain trace health conditions (n=360) | ||
| No | 181 | 50.3 |
| Yes | 179 | 49.7 |
| Reported usual use of injectable medications given per tracer conditions # or not included in EDL | ||
| Analgesics | 77 | 43.0 |
| Antibiotics | 64 | 35.8 |
| H2 blockers | 19 | 10.6 |
| Corticosteroids | 15 | 8.4 |
| Antispasmodics | 4 | 2.2 |
Table 1: Pattern of injection usage in primary health care facilities of Idku city.
Nearly a third of PHC physicians (31.6%) examined more than 100 patients per week. Most of the physicians (80.3%) made prescriptions that included at least one injection for less than 10 patients seen. The majority of physicians (93.4%) perceived that number of injections prescribed was reasonable. More than half of the physicians (52.6%) prescribed injections to treat dental abscess. The injectable medications that are often prescribed by the physicians were the antibiotics (56.6%). More than two fifths (43.4%) of physicians stated that their patients prefer injections over oral medications (Table 2).
| Variable | Injection prescriber (n=76) | |
|---|---|---|
| No. | % | |
| The average number of patients per week/physician | ||
| Less than 50 | 33 | 43.4 |
| 50-100 | 19 | 25.0 |
| More than 100 | 24 | 31.6 |
| The average number of prescriptions include injection/physician/week | ||
| Less than 10 | 61 | 80.3 |
| 10-20 | 13 | 17.1 |
| 20-50 | 2 | 2.6 |
| Physician perception about the frequency of injection use | ||
| Accepted | 71 | 93.4 |
| Too many | 5 | 6.6 |
| The diseases for which injections prescribed most often | ||
| Acute follicular tonsillitis | 16 | 21.1 |
| Respiratory tract infection | 5 | 6.6 |
| Gastrointestinal diseases | 6 | 7.9 |
| Dental abscess | 40 | 52.6 |
| Gynecological and Obstetric diseases | 7 | 9.2 |
| Acute otitis media | 2 | 2.6 |
| The injectable medications prescribed most often | ||
| Antibiotic | 43 | 56.6 |
| Analgesic | 21 | 27.6 |
| Antiemetic | 6 | 7.9 |
| Hemostatic | 6 | 7.9 |
| The preferred type of medications from the side of the patient | ||
| Injections | 33 | 43.4 |
| Oral or other non-injected medications | 33 | 43.4 |
| Either | 10 | 13.2 |
Table 2: Injection pattern of use as reported by physicians of PHC facilities of Idku city.
Injection provider interview
The average number of injections given per day by the injection providers ranged from 2 to 30 injection with a median of 6 (IQR=3.7) injections. The majority of the injection providers (88.2%) gave less than 10 injections per day. Only 8.6% of injection providers think that they give too many injections.
Recipients’ experience regarding injection
During the last 3 months preceding the study, nearly 80.4% of studied service consumers received injections. Of those, the majority (92.6%) was for therapeutic purpose or for contraception. Vast majority of the injection recipients (97.3%) think that they take too many injections. The last injection for three quarters of recipients was given by non-medical personnel outside the facility. Less than a third of the recipients prefer (29.9%) prefer injections.
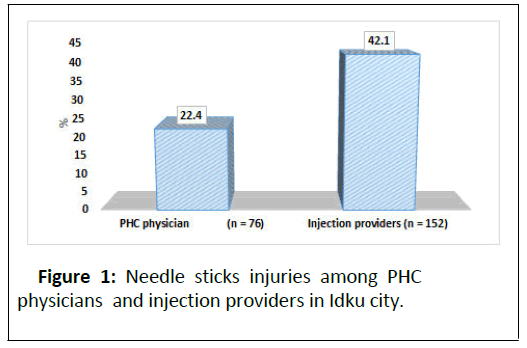
Health care workers perspectives about injection safety practices, and hazards
Only 40.8% of the physicians and 38.2% of the injection providers got training regarding injection safety within the last 2 years. The majority of physicians and injection providers (85.5% and 88.25 respectively) received three doses of hepatitis B vaccine. More than one fifth of the studied physicians (22.4%) and 42.1% of the injection providers had Needle Stick Injuries (NSIs) in the last 6 months preceding the study. Of the physicians, nearly two thirds (64.7%) reported the incidents and they know to whom they report (the main reasons stated for not reporting were time constraint, no reporting channel, and low perceived risk of disease transmission due to incident). Of those reported the NSIs, more than half (54.5%) received counseling and a similar proportion offered disease testing. However, the majority (90.9%) were not provided with any post exposure prophylaxis. Of those injection providers who experienced NSIs, more than three-quarters (76.6%) reported the injuries. Most of the providers (81.2%) know to whom they report the NSIs. Of those reported the NSIs, more than two thirds (69.4%) received counseling and more than half (55.1%) offered disease testing. However, 79.7% of them were not provided with any post exposure prophylaxis. Only 24.3% claimed that they have guidelines for post exposure prophylaxis (Figure 1).
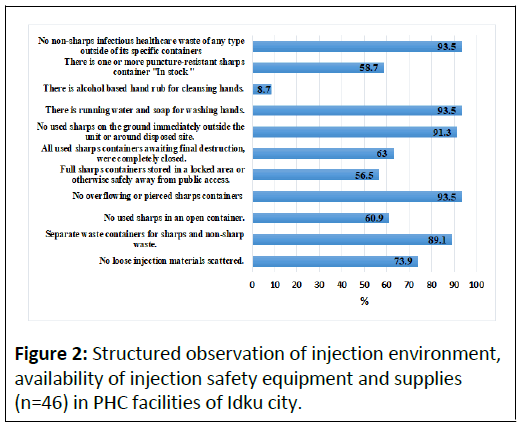
Structured observation of equipment and supplies
A total of 46 locations were observed in the 12 health facilities visited namely; emergency units (n=12), family planning clinics (n=12), vaccination rooms (n=12) and dental clinics (n=10) in order to systematically assess safe injection and disposal equipment and supplies at the facility. Illustrates, items that were met in very high proportions in the observed settings were; availability of separate waste containers for sharps and non-sharp waste (89.1%), no overflowing or pierced sharps containers (93.5%), no used sharps on the ground immediately outside the facility or around the disposed site (93.5%) and no non-sharps infectious healthcare waste of any type outside of its specific containers (93.5%) (Figure 2).
However, items met in lower proportions of PHC settings were; no loose injection materials scattered (73.9%), no used sharps in an open containers (60.9%). In 63.0% of instances, all used sharps containers awaiting final destruction were completely closed. In more than half of the injection settings there were one or more puncture-resistant sharps container “in stock” (58.7%), and full sharp-containers stored in a locked area or otherwise safely away from public access were met (56.5%). The item that is least met was that availability of alcohol based hand rub for cleansing hands (8.7%).
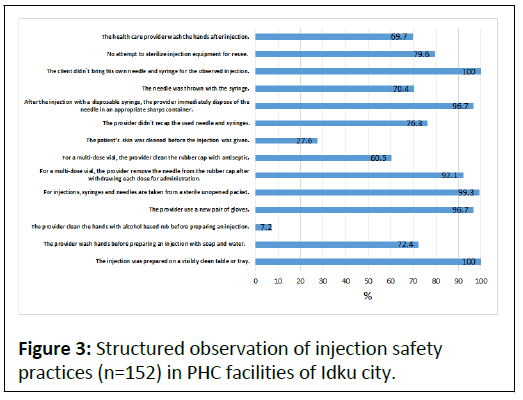
Structured observation of injection safety practices
A total of 152 injection events were observed in 4 areas at each PHC facility namely; emergency unit (n=36), family planning clinic (n=38), vaccination room (n=38) and dental clinic (n=40) in order to systematically assess the injection safety practices at the facility. The items that were met in very high proportions in the observed injection events were; the injection was prepared on a visibly clean surface (100.0%), the provider use a new pair of gloves (96.7%), syringes and needles are taken from a sterile unopened packet (99.3%), for a multi-dose vial, the provider remove the needle from the rubber cap after withdrawing each dose for administration (92.1%), after the injection with a disposable syringe, the provider immediately dispose of the needle in an appropriate sharps container (96.7%) and no clients bring his/her own needle and syringe for the observed injection (100.0%) (Figure 3).
The injection safety practices observed in lower proportions were the following; the provider wash hands before preparing an injection with soap and water (72.4%), for a multi-dose vial, the provider clean the rubber cap with antiseptic (60.5%), the injection provider didn’t recap the used needle and syringes (76.3%), the needle was thrown with the syringe (70.4%), the health care provider didn’t has any attempt to sterilize injection equipment for reuse (79.6%), the health care provider wash the hands after injection (69.7%).
The least observed practices were; the patient’s skin was cleaned before the injection was given (27.6%) and the provider clean the hands with alcohol based rub before preparing an injection (7.2%).
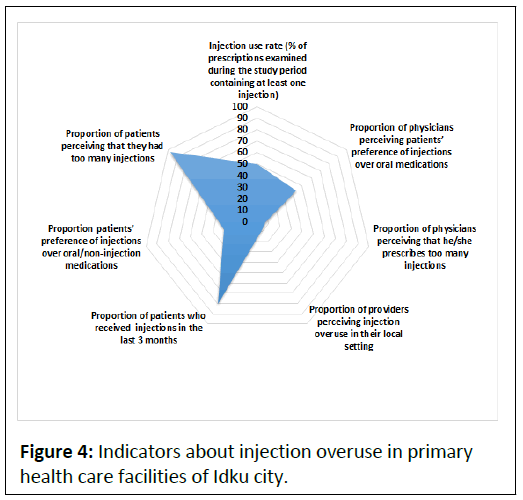
Facility speci fic indicators for inject ion over use and inject ion safety in Idku city
Injection use rate (defined as % of prescriptions examined containing at least one injection) was 50.0% (95% CI=42.8-61.9). Out of 76 physicians interviewed, 43.4% perceived patients’ preference of injections over oral medication. Furthermore, 6.6% of the physicians perceived that they prescribe too many injections. About 13 of the 152 injection providers (8.6%) perceived injection overuse in their local setting.
The ratio of therapeutic to immunization injections at the PHC facilities of Idku was 137:11 (90.0%). High proportion of patients (80.5%) received injections in the last 3 months preceding the study. Less than a third of patients (29.9%) prefer injections over oral or non-injection medications. Vast majority of patients (97.3%) perceived that they had too many injections (Figure 4).
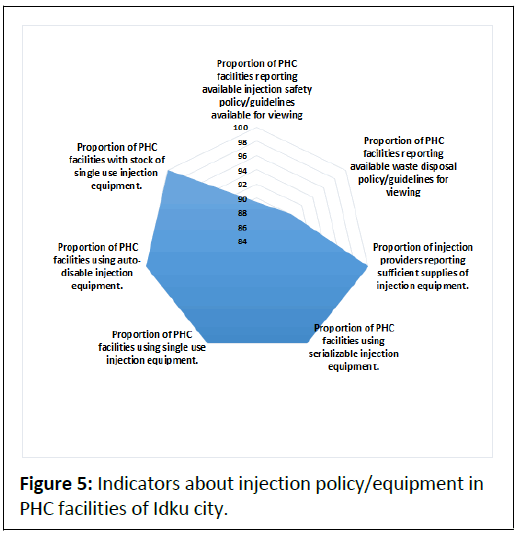
Vast majority of the facilities showed availability of injection safety policy/guidelines (89.5%) and waste disposal policy/ guidelines for viewing (90.1%). All of the injection providers reported sufficient supplies of injection equipment. All of the facilities showed using of sterilized injection equipment; single use injection equipment and auto disable injection equipment. In addition, all of the facilities have stock of single use injection equipment (Figure 5).
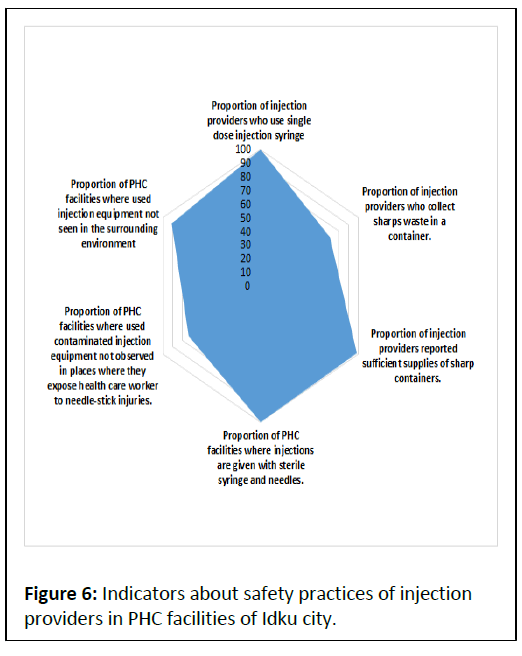
Of the 152 injection safety practices observations, none of the injection providers used reusable injection equipment. Nearly three-quarters of them (71.1%) collected sharp waste in a container. In all of the 152 observations, injections were given with sterile syringes and needles. Vast majority of the injection providers (98.7%) reported sufficient supplies of sharp containers. More than half (53.9%) reported access to sharp waste disposal facility. Injection safety equipment observations (n=46) indicated that, in 26.1% of instances, used contaminated injection equipment can be observed in places where they expose health care workers to NSIs and in 8.7% of instances, used injection equipment can be seen in the surrounding environment (Figure 6).
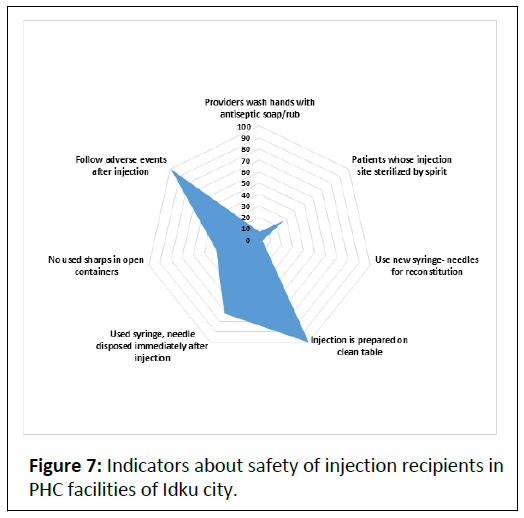
In the 152 injection events, only 7.2% of injection providers washed their hands with antiseptic soap or used alcohol based rub. More than fourth injection providers (27.6%) cleaned or wiped the injection site with rectified spirit before providing injections.
In a minority (2.6%) % of all injections being administered (n=152), the injection providers used new syringes and new needles for reconstitution.
In all of the 152 injection events, the injection providers always prepare the injections on a clean table or tray and follow up the adverse events after injection. Used syringes and needles were disposed immediately after injection by 71.7% of the injection providers. In 39.1% of observed events, no used sharps seen in an open containers (Figure 7).
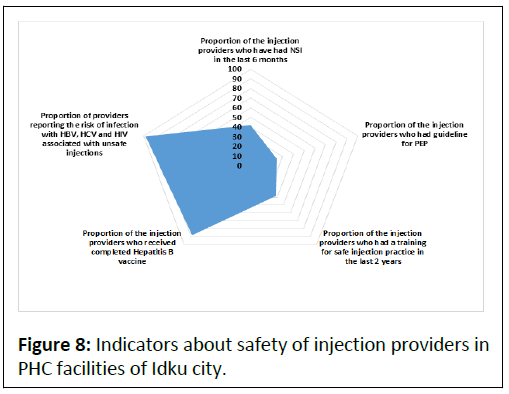
Needle-stick injuries were common with 42.1% of the injection providers in PHC facilities reporting having had such injuries in the last six months before the survey. Only one fourth of injection providers (24.3%) had guidelines for Post Exposure Prophylaxis (PEP). Slightly more than a third of them (38.2%) had training in injection safety practices in the last 2 years. On further assessment concerning the safety of the injection providers, it was found that the majority of injection providers (88.2%) were fully immunized against hepatitis B virus (all 3 doses completed). Almost all, n=149 (except one) of the studied injection providers reported the risk of HBV, HCV and HIV associated with unsafe injections (Figure 8).
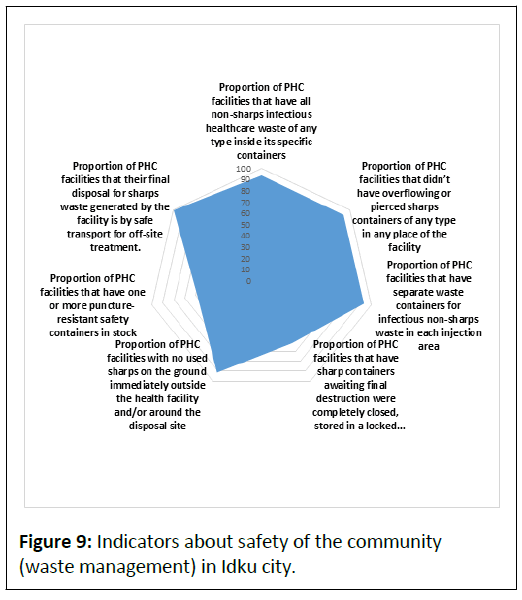
According to observation of injection settings (n=46), in the majority of settings (93.4%), there were non-sharps infectious healthcare waste inside their specific containers. A similar proportion (93.4%) did not have overflowing or pierced sharp containers in some places in the facility. In 93.5% of instances, there were separate waste containers for infectious non-sharp waste in each injection area. In less than two-thirds of the settings (62.2%), sharp containers waiting for final destruction were completely closed, stored in a locked area safely from public access (Figure 9).
In the majority of the settings (91.3%), there were no used sharps have been seen on the ground immediately or around the disposal site. In more than half of the settings (58.7%), there were one or more puncture resistant safety containers in stock. All of the head nurses at the PHC facilities reported that their final disposal for sharp waste generated by the facility is by transport off-site for treatment.
Discussion
This is the first study that depicts the extent and characteristics of injection use and injection practices in PHC facilities of Idku city. The information is being used to design and evaluate interventions to promote safe injections in PHC settings. This certainly provides information to identify weak areas in order to improve further the national guidelines. A first step toward evaluating the frequency of unsafe injection practices in countries is an injection safety assessment three major contemplations are particularly important in the assessment of potential unsafe injections. The safety of the recipient, the safety of the healthcare workers and the safety of the community. In this study, data were obtained by combination of different methods; prescription reviewing, interviews and structured observations. In this way we attempted to overcome bias due to missing data, reporting bias and the Hawthorne effect (observer-induced changes in practices) [14].
The advent of injections into medicine remains excellent points of interest. However, the inappropriate and/or abuse of injections are recognized public health challenges, globally. Carrying untoward effects on people and health systems, this danger has remained unnoticed at the primary level of healthcare [15].
Injections are frequently used unnecessarily when oral medicine could be equally effective. WHO handbook for good prescription has recommended that less 10% of outpatient prescriptions should contain injectable drugs [16]. In the present study, injection use rate was 50.0% which exceeds the reference value recommended by the WHO. This observance of higher injection use in PHC facilities is consistent with a study conducted in primary health care hospitals in Bangladesh that has found very high rates of unnecessary or avoidable use of injections (60%-80%) [17].
The WHO fact book reported an injection use rate of 27.5 % which is lower than that attained in this study [18]. Our result also demonstrated a higher use of injectable medications when compared to results reported for Eastern Mediterranean (20.1%), European (17.2%) and West Pacific (23.2%) regions. Indiscriminate use of injections can increase the chance of spreading blood-borne diseases such as hepatitis B and even HIV/AIDS particularly in a region where infections rates remain high. Moreover, overuse of injections sets up a cycle of repeated visits putting pressure on healthcare staff and driving costs [19]. In contrary, higher injection use rate of 79.1% was reported in 2018 who explored the pattern of injections usage in rural PHC facilities in north-western Nigeria [15].
The observance that the bulk of injections provided in Idku are therapeutic and administered mostly by untrained informal providers presents a challenge for behavior change strategies to minimize overuse of injections and promote injection safety. The prescribers should be provided with clear prescription policy advocating for rational prescription of injections. Health education communication strategy targeting prescribers and providers to promote safe injections must incorporate both knowledge base and behavior change components [20]. The finding that people can get injections from non-medical staff emphasizes also the significance of increasing awareness of the public about the injection safety. The administration of injections regularly requires frequent supervision by skilled health care providers. Community health education is essential focusing on consumer demand for injections and creating public demand for safe injections and safe medical procedures [21]. Moreover, a community based study is required to explore the role and impact of sizable informal injection providers.
In this study, 43.4% of physicians perceived that their patients prefer injections over oral medications and 29.9% of the recipients told that they prefer injections which exceed the national standard of WHO (<15%) [22]. A systematic review indicated that patient preference and socio-cultural beliefs have been noted to influence prescribing behaviour [23]. Reasons of injection overuse were reported in a study in Tanzania [24]. Some patients more inquire for prescribing injections because they believed injections were more-stronger and faster medications, outwit the issues of having to swallow terrible tasting tablets and stomach upsets caused by pills, and because they are particularly useful for children who are always hesitant to swallow oral medication. Clinicians may contribute to this increased frequency of injections use by assembly patients’ request for injections and getting indirect benefit for prescribing injections by keeping their patients. Effective communication between patients and providers can clarify these misunderstandings and reduce injection overuse [25].
Prescription reviewing revealed that the use of injectable analgesics (43.0%) was more frequent than that of injectable antibiotics (35.8%). Prescribers’ interviews revealed that the injectable medications that are frequently endorsed by the physicians were the antibiotics (56.6%). Both results surpass the reference value (<30%) recommended by the WHO [22]. This might be attributed to lack of in-service training. Bangladesh study reported that the foremost prescribed injectable medications were antibiotics, intravenous fluids, and analgesics, respectively [26]. At PHCs, laboratory facilities are often nonexistent and as such prescribers may depend primarily on their clinical judgment. Whereas empirical use of antibiotics based on clinical judgment other than laboratory confirmations is permitted in numerous occasions such as otitis, apparent pneumonia and cellulitis, it is well recognized that consistent use of antimicrobials when infection or diagnosis has not been established or completely affirmed can lead to overprescribing. Indiscriminate use of antibiotics supported by no diagnostic certainty can contribute to the development of drug resistance [27]. A further qualitative research is required to investigate reasons for patients’ demand for injections and motivations for over-use of injections among health care providers.
Needle-stick injuries in health-care workers are nearly totally preventable by improving workplace practices, but when they do happen the consequences for the individual can be serious, regardless of the outcome in terms of infection [28]. In the present study, NSIs were experienced among 22.4% of the studied physicians and 42.1% among the injection providers. A study reported comparable prevalence of 31.2% in Ilorin, Nigeria among HCWs in primary health facilities [29].
Injection safety equipment observations indicated that, in 26.1% of occasions, used contaminated injection equipment can be watched in places thus exposing health care workers to NSIs, thus exposing the health care workers to the risk of infection of blood-borne pathogens [30]. Our study provides expressive epidemiological evidence of how such injuries happen. Results from this study indicated that 2-handed recapping occurred in 23.7% of injections and manual removal of needles occurred in 29.6% of injections, all are against MOHP policy of injection safety. Tendency to recap the needle increases when safety boxes are kept distant from the injection location [31]. In our study, only 53.9% of the injection providers reported accessibility to sharp boxes. Decreases in NSI rates may well be achieved by performing fewer injections and cessation of 2- handed recapping of needles or using the one-handed scoop technique. There is a need to reaffirm MOH policies and for solid and sustained supervisory action to prevent injection-associated infections.
Provision of Post Exposure Prophylaxis (PEP) is essential for health care workers’ safety. Our study revealed that most of the studied health care facilities lacked PEP practices. Absence of a guideline for Post Exposure Prophylaxis (PEP), no formal system for reporting, leaves the injection providers to manage NSI on their own. Post-exposure management includes first aid, serological testing and counseling in all cases. Immune prophylaxis and antiviral medications are used in some cases. Advice and guidance ought to continuously be looked from local specialist services [32].
Immunization of HCWs for HBV, and providing training to HCWs in safe injection practices to increase awareness and encourage behavioral change, are effective interventions that could avoid NSI and its consequences [33]. In our study 85.5% of the injection providers had been vaccinated against hepatitis B with three doses, In United Kingdom 90%, a figure that was comparable to that found in our study. However, in the present work, there was a lack of training of all interviewed primary care workers on distinctive practices related to safe injection. Comparative results were reported in Gharbiya governorate, Egypt [34,35].
Observations in all PHC facilities demonstrated the universal use of single-use, disposable syringes and needles for injections. These findings correlate with studies conducted in Swaziland, and Ethiopia. Use of single-use injection equipment syringes and needles may be due to satisfactory availability and supply.
Results of this study showed that few of the health-care facilities studied considered needed policies and guidelines imperative for safe injection practices and safe disposal. In contrary, a study carried out in Nepal 2016 found that a few supervisors (6%) claimed to have guidelines for safe injection practice and they were not able to produce this when requested. Similarly in Bangladesh, none of the health facilities (n=24) observed, had injection safety and waste disposal policy or guidelines available for viewing. However, in India, 14.2% of health facilities observed had guidelines for waste disposal.
Understanding injection practices is crucial for evidencebased development of intervention initiatives. In the current study, there was huge scope for improvement of some poor components of injection practices in the PHC facilities. Hand hygiene before injection preparation and after injection, cleaning rubber cap with antiseptic in case of multi dose vial, recapping of the used needle, the needle should be thrown with the syringe, no reusing of injection equipment, patient’s skin preparation and disinfection before injection and hand rub with alcohol before preparing an injection all need to be revised. It is suggested that there should be on-job training and regular supportive supervision of the staffs on proper injection procedures, and proper usage of available injection equipment.
Safe sharps waste management is essential for safety of the community. In spite of the fact that the amount of sharps waste generated in primary health care facilities is very small (nearly 1%), the hazards associated with them should not be neglected. Waste disposal practice in primary health care facilities in Idku was not satisfactory. Despite the high availability and adequate supply of injection safety box, used syringes and needles were not disposed immediately after injection; used sharps were seen in open containers and overfilling of safety boxes were also seen in some locations. In addition, sharp containers awaiting for final destruction were not totally closed, and stored near to public access. Typically comparable to reports from Burkina Faso and Dominican Republic. This finding showed that availability of injection equipment does not necessarily result in proper usage of this equipment and this buttressed the need for strong supervision for primary health care workers. In this study, training is needed of all health-care personnel with respect to segregation practices. Training of waste workers should involve safe handling, storage and operation and maintenance of treatment technologies. Written instructions should be available for waste workers with adequate and regular supervision.
As far as the patients and providers' safety is concerned, this study demonstrated a need for further research exploring the dynamics of injection use and safety in Idku. In a context where a high level of injection use and unsafe practices were reported, immediate prevention activities need to be operated through continued intervention efforts and health providers' training in primary care facilities of Idku.
Conclusion
Safe injection practices are part of standard practices in health care delivery aimed at keeping up basic levels of patient safety and provider protection. In the present study, the frequency of injections in primary health care facilities in Idku is high. In addition, unsafe injection practices were noted. Strategies for rational use of injections should be carefully implemented to avoid decrease of necessary injections. Interventions should involve the prescribers, the injection providers, and the general population. The physicians should consider prescribing fewer unnecessary injections and injection providers should all receive HBV vaccination and trained properly on safety practices. The general population must become more aware of the consequences of unnecessary and unsafe injections. More research is required to understand the problem and to develop evidence based interventions.
Limitation of the study
Because our study focused on primary health care facilities of Idku city, our findings and conclusions may not be representative of other health care settings including hospitals, and private practices of Idku. The possibility of reporting bias is very high in the reported needle stick injuries; the main reasons stated for not reporting were time constraint and low perceived risk of disease transmission due to incident.
References
- Hayashi T, Hutin YF, Bulterys M, Altaf A, Allegranzi B (2019) Injection practices in 2011-2015: A review using data from the Demographic and Health Surveys (DHS). BMC Health Serv Res 19: 600.
- Kane A, Lloyd J, Zaffran M, Si monsen L, Kane M (1999) Transmission of hepatitis B, hepatitis C and human immunodeficiency viruses through unsafe injections in the developing world: Model-based regional estimates. Bull World Health Organ 77: 801-807.
- Hauri A, Ar mstrong GL, Huti n YJF (2003) Contaminated injections in health care settings. In: Ezzati M, Lopez AD, Rodgers A, Murray CJL. Comparative quantification of health risks: Global and regional burden of disease attributable to selected major risk factors. Geneva, World Health Organization.
- World Health Report (2002) Preventing risk factors, promoting healthy life. Geneva.
- Nili T, Amal MS, Shaul SS (2006) The health beliefs of hospital staff and the reporting of needlestick injury. J Clin Nurs 15: 1228-1239.
- Nagao Y, Baba H, Torii K, Nagao M, Hatakeyama K, et al. (2007) A long term study of sharps injuries among health care workers of Japan. Am J Infect Control 35: 407-411.
- World Health Organization (WHO) (2008) Revised injection assessment tool (tool C revised). Geneva: Geneva, Switzerland.
- Bodenschatz C, Talaat M, Kandeel A, Lohiniva AL, Radwan E, et al. (2009) Injection prescribing patterns in public health care facilities in Egypt. East Mediterr Health J 15: 1440-1448.
- Talaat M, El-Oun S, Kandeel A, Abu-Rabei W, Bodenschatz C, et al. (2003) Overview of injection practices in two governorates in Egypt. Trop Med Int Health 8: 234-241.
- Gyawali S, Rathore DS, Shankar PR, Kc VK, Jha N, et al (2016) Knowledge and practice on injection safety among primary health care workers in Kaski District, Western Nepal. Malays J Med Sci 23: 44-55.
- Omole VN, Joshua IA, Muhammad-Idris ZK, Usman NO, Ahmad IA (2018) Use of injections and antibiotics and profile of health workers in rural primary health care facilities in North-western Nigeria. 23: 183-188.
- Hogerzeil HV, Barnes KI, Henning RH, Kocabasoglu YE, Moller H, et al. (2001) Teacher’s guide to good prescribing. World Health Organization (WHO), Department of essential drugs and medicines policy, Geneva, Switzerland.
- Chowdhury AKA, Rahman SM, Faroque ABM, Hasan GA, Zahir Raihan SZ (2007) Wide spread injection use in the hospitals of the upazila health complexes of Bangladesh. Mymensingh Med J 8: 123-131.
- Isah A, Ross-Degnan D, Quick J, Laing R, Mabadeje A (2001) The development of standard indicator values for the WHO drug use prescribing indicators.
- Ofori-Asenso R, Agyeman AA (2015) A review of injection and antibiotic use at primary health care (public and private) centers in Africa. J Pharm Bioallied Sci 7: 175-180.
- Gyawali S, Rathore DS, Shankar PR, Kumar KV (2013) Strategies and challenges for safe injection practice in developing countries. J Pharmacol Pharmacothe. 4: 8-12.
- Enwere OO, Diwe KC (2014) Knowledge, perception and practice of injection safety and healthcare waste management among teaching hospital staff in south east Nigeria: An intervention study. Pan Afr Med J 17: 218.
- Ofori-Asenso R., Brhlikova P, Pollock AM (2016) Prescribing indicators at primary health care centers within the WHO African region: A systematic analysis (1995-2015). BMC Public Health 16: 724-738.
- Massele AY, Mwaluko GM (1994) A study of prescribing patterns at different health care facilities in Dar es Salaam, Tanzania. East Afr Med J 71: 314-316.
- Meskarpour-Amiri M, Dopeykar N, Mehdizadeh P, Ayoubian A, Motaghed Z (2015) A study on the factors affecting the prescription of injection medicines in Iran: A policy making approach. Glob J Health Sci 7: 291-297.
- Chowdhury AA, Roy T, Faroque A, Bachar S, Asaduzzaman M, et al. (2011) A comprehensive situation assessment of injection practices in primary health care hospitals in Bangladesh. BMC Public Health 11: 779.
- Llor C, Bjerrum L (2014) Antimicrobial resistance: Risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf 5: 229-241.
- Bowden FJ (2001) Needle-stick injuries in primary care. Aust Prescr 24: 98-100.
- Bolarinwa OA, Asowande A, Akintimi CI (2011) Needle stick injury pattern among health workers in primary health care facilities in Ilorin, Nigeria. Acad Res Int 1: 419-427.
- Perry J, Jagger J, Parker G, Phillips EK, Gomaa A (2012) Disposal of sharps medical waste in the United States: Impact of recommendations and regulations, 1987-2007. Am J Infect Control 40: 35-58.
- Ribner BS, Landry MN, Gholson GL, Linden LA (1987) Impact of a rigid, puncture resistant container system upon needle-stick injuries. Infect Control 8: 63-66.
- Fitz Simons D, Francois G, De Carli G, Shouval D, Pruss-Ustun A, et al. (2008) Hepatitis B virus, hepatitis C virus and other blood-borne infections in health care workers: Guidelines for prevention and management in industrialized countries. Occup Environ Med 65: 446-451.
- Ismail NA, Aboul Ftouh AM, El-Shoubary WH, Mahaba H (2007) Safe injection practice among health-care workers in Gharbiya Governorate, Egypt. East Mediterr Health J 13: 893-906.
- Daly A, Nxumalo M, Biellik R (2008) An assessment of safe injection practices in health facilities in Swaziland. SAMJ 94: 194.
- Zewdie A, Wabe NT (2012) The prevalence of therapeutic injections in Ethiopia: From the patients’ and health care providers’ perspectives. Gaziantep Med J 18: 21-26.
- Chowdhury AKA, Roy T, Faroque ABM, Bachar SC, Asaduzzaman M, et al. (2011) A comprehensive situation assessment of injection practices in primary health care hospitals in Bangladesh. BMC Public Health 11: 779.
- IPEN Study Group (2012) Injection practices in India. WHO South-East Asia J Public Health 1: 189-200.
- Pruss A, Giroult E, Rushbrook P (1999) Safe management of waste from health care activities. Geneva: World Health Organization.
- Fitzner J, Aguilera JF, Yameogo A, Duclos P, Hutin YJ (2004) Injection practices in Burkina Faso in 2000. Int J Qual Health Care 16: 303-308.
- Moro PL, Moore A, Balcacer P, Montero A, Diaz D, et al. (2007) Epidemiology of needlesticks and other sharps injuries and injection safety practices in the Dominican Republic. Am J Infect Control 35: 552-559.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences