Baseline Characteristics of a Cluster Randomized Controlled Trial on the Effectiveness of a Multi-Component Intervention in Promoting Healthy Diet and Physical Activity in Adults with Diabetes in Oman
Thuraiya Al Harthi1*, Thamra Al Ghafri2, Fathiya Al Jufaili3, Amjad Al Ghammari4, Nawal Al Haddabi4, Safia Al Araim4, Aiysha Al Riyami4, Sameera Al Bulushi4, Hanan Al Kindi4, Huda Al Kaiyumi4, Sumaiya Ambusaidi4, Shamsa Al Harthi5, Huda Anwar6
1Department of Epidemiology, Directorate General of Health Services of Muscat Governorate, Oman, Muscat
2Department of Family Medicine, Directorate General of Health Services of Muscat Governorate, Oman, Muscat
3Department of Nutrition, Directorate of primary health care. Directorate General of Health Services of Muscat Governorate, Oman, Muscat
4Department of Clinical Nutrition, Directorate of primary health care, Oman, Muscat
5Department of School and University Health, Directorate General of Primary Health Care, Oman, Muscat
6Department of Primary Health Care, Director of Primary Health Care of Muscat governorate, Oman, Muscat
*Corresponding Author:
- Thuraiya Al HarthiDepartment of Epidemiology, Directorate General of Health Services of Muscat Governorate, Oman, Muscat E-mail: thuraiya.alharthi@moh.gov.om
Received date: April 2, 2022, Manuscript No. IPJPM-22-13065; Editor Assigned date: April 4, 2022, PreQC No. IPJPM-22-13065(PQ); Reviewed date: April 19, 2022, QC No. IPJPM-22-13065; Revised date: April 25, 2022, Manuscript No. IPJPM-22-13065(R); Published date: May 2, 2022, DOI: 10.36648/2572-5483.7.5.139
Citation: Al Harthi T, Al Ghafri T, Al Jufaili F, Al Ghammari A, Al Haddabi N, et al. (2022) Baseline Characteristics of a Cluster Randomized Controlled Trial on the Effectiveness of a Multi-Component Intervention in Promoting Healthy Diet and Physical Activity in Adults with Diabetes in Oman. J Prev Med Vol.7 No.5:139
Abstract
Objective: A post hoc analysis, describing the baseline characteristics and evaluating comparability of comparison groups in an ongoing trial that aims in measuring the effectiveness of multi-modality intervention in promoting healthy lifestyle in patients with diabetes.
Design: Cluster randomized controlled trial.
Setting: Eight primary care centers in Muscat governorate.
Participants: 589 adults with diabetes following up for 12 months, randomized to intervention and control group. Intervention: Using motivational interview techniques, virtual consultations, and pedometer bands for step count compared with standard usual care in primary health centers.
Main outcome measure: The overall frequency of baseline covariable and the unadjusted mean difference in glycemic parameters.
Results: 285(48.4%) were assigned to intervention and 304(51.6%) to the control arm, randomly. Overall, 59% of participants were female, median age was 47(interquartile range (IQR=55-41) years old, 359(61.0%) had body mass index equivalent or above 30 kg/m2, 214(36.3%) of males had a Waist Circumference (WC) equivalent or above 94 cm, and 337(96.8%) of females with WC equivalent or above 80 cm. Mean difference in glycemic parameters between intervention group vs control was -0.44%(95% CI: -0.75 to 0.14) for glycated hemoglobin, - 3.5 kg/m2(-5.0 to 1.8) for body mass index, -4.2 cm(-6.3 to 2.1) for waist circumference, 0.10 g/dl(-0.2 to 0.1) for low density lipoprotein cholesterol, and -0.01 g/dl(-0.07 to 0.04) for high density lipoprotein. The difference in median systolic and diastolic blood pressure had a p-value of 0.125 and 0.162, respectively.
Conclusion: The baseline characteristics of the study cohort showed that most patients with diabetes were obese with central obesity predominant in females. Statistical analysis suggests between group comparability at baseline, however, proper randomization, predetermined eligibility criteria, and baseline covariables are the mainstay to ensuring balance between study arms at baseline.
Introduction
The global prevalence of Diabetes Mellitus (DM) for 2015 and 2040 was estimated to be 8.8% among adults aged between 20 and 79 years old [1]. The epidemiological surveys have shown the increasing trends of diabetes over recent decades with dramatic increase in developing countries including the MENA region [2-5]. The consequent burden of diabetes care and management on healthcare system necessitates serious actions towards disease control and prevention.
In Oman, 15.7% of people are diagnosed with diabetes and 11.8% are prediabetes, according to a community-based survey, which also showed high prevalence of diabetes risk factors including behavioral factors [6]. The national institute of health metrics and evaluation has reported diabetes as the sixth leading cause of premature death and the fifth cause of disability-adjusted life years lost [7]. Thus, the ministry of health directed its effort towards planning strategies and implementing policies for diabetes control and management.
Physical inactivity is estimated to be an attributing cause to 27% of diabetes, and 30% of ischemic heart disease [8]. Similarly, greater sitting time known as Sedentary Behavior (SB) is considered an independent risk factor for diabetes, cardiovascular disease, and all-cause mortality [9,10]. Sitting more than 8h/day leads to increase risk of all-cause mortality even among those achieving the recommended 150 min/week of moderate to vigorous Physical Activity (PA) [11].
Obesity considered the fifth leading cause of mortality worldwide and an independently risk factor for multiple chronic diseases including diabetes, cardiovascular and hepatocellular diseases [12,13]. The burden of obesity and overweight are substantial across the globe, including the economic burden, where in 2019 the cost has been estimated to range from US$17 in India to US$940 in Australia [14].
In Oman, over the past few years, sufficient evidence on diabetes risk factors surveillance were published, however, research on intervention and prevention programs for healthy behavior promotion are scares [6,15].
The protocol for the current study was published in 2020 which aimed at measuring the effectiveness of utilizing motivational interview, telemedicine based consultations, and pedometer in promoting for physical activity and healthy diet among patients with diabetes receiving care in primary health centers, over 12 months period [16].
In this paper present the findings of the post hoc analysis for the baseline data that was collected between October 2021 and January 2022 for the ongoing randomized control study [16]. We describe the baseline sociodemographic and clinical characteristics of the comparison groups and measure their comparability.
Methods
Study setting
Eight primary care facilities were randomly assigned to intervention and control groups, using random numbers table generated via STATA 16.
Study population
700 participants (375 in each arm) with diabetes who have visited the diabetes clinic in primary care health facility within the last 6 months before the study onset.
Patients were identified through the electronic medical record “Al-Shifa”-Diabetes clinic patient list.
Included patients were adults aged between 18 and 65 years, physically inactive with no contraindication to physical activity, not on a restricted diet, able to speak and read Arabic, willing and able to provide written informed consent, and can use phone applications.
Patients with clinical conditions that are mandates refrain from physical activity and normal healthy diet (Appendix 1) were excluded. We also excluded those who did not have easy access to internet connections.
Randomization and recruitment
Detail on randomization process and recruitment are found in the study protocol published elsewhere [16].
Intervention group (exposure)
375 patients are assigned to receive motivational interview-based counselling, virtual follow up consultations through educational e-messages and audiovisual consultations, and pedometer wrist bands to trace steps and activity level.
Control group
375 patients are assigned to receive standardized usual care provided in health centers.
Outcome of interest
Primary outcome: Comparison of the baseline characteristics that pronounce patients’ initial demographic, clinical, and healthy lifestyle, between the intervention and control group. Socio-demographic information is represented by age and sex.
The clinical (glycemic) parameters of interest are weight, BMI, waist circumference, glycated hemoglobin (HbA1c), Low Density Lipoprotein Cholesterol (LDL-C), High Density Lipoprotein Cholesterol (HDL-C), systolic and diastolic blood pressure.
Healthy lifestyle is quantified by measuring number of steps achieved using pedometer bands and energy expenditure in the last 7 days using GPAQ. Macronutrient intake of calorie, carbohydrate, protein, and fat is also measured using FFQ questionnaire, conducted face-to-face by the dietician.
Secondary outcome: Frequency of patients according to stages of behavior change and reasons against change are also determined during counselling conducted by the dietician.
Further information is found in this study protocol, where link in given elsewhere in this manuscript.
Statistical Analysis
Descriptive analysis was reported using mean and Standard Deviation (SD), median with Interquartile Range (IQR), and count with percentage. To compare between the two groups, we calculated the mean difference in baseline characteristics reported in this trial using t-test for continuous variables that are normally distributed. For non-normally distributed (i.e., nonparametric), Wilcoxon rank-sum test was used. Chi square test was used to examine the variability of behavior change stages and barriers to change in both arms. Missing data were imputed by the mode value (the most frequent value). We followed the CONSORT statement in reporting the baseline findings of this paper [17]. Stata version 16 was used to conduct the analysis.
Results
Study population
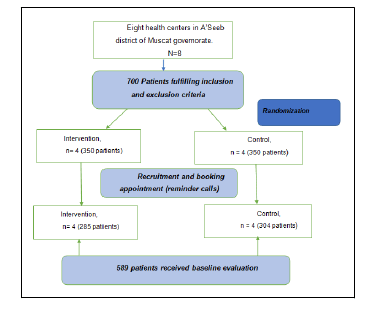
700 patients were reached through phone call and given an appointment to attend the baseline assessment and care on a specific day at patients’ convenience. 350 patients were recruited in each arm. After several reminder call, eventually 589 participants attended their appointments where written consent was provided by 304 patients in the control group and 289 in the intervention, who visited the clinic in person. Figure 1 shows patients’ flow throughout the recruitment and baseline assessment phase (Figure 1).
241(~ 41%) were male participants and median age was 47 (IQR=55-41) years old. Mean HbA1c was 7.8 (1.9)%, mean weight was 83.6 (47.2) Kg, mean BMI 33 (9.9) Kg/m2, mean waist circumference was 106.1 (12.2) cm in males and 104.4 (13.6) in females, median systolic and diastolic blood pressure were 134(IQR=149-124) and 80(88-72) mmHg, respectively, and mean LDL and HDL cholesterols were 2.9 (0.9) and 1.2(0.4), respectively, which indicates above target levels for lipid control according to national guidelines.
373 (63.3%) participants had an HbA1c equivalent or above 7%, 359 (61.0%) with BMI equivalent or above 30 kg/m2, 530 (90%) with an LDL-cholesterol equivalent or above 1.8 mmol/l, 126 (21.4%) with HDL-cholesterol less than 1 mmol/l, 214 (36.3%) of males had a waist circumference equivalent or above 94 cm, and 337 (96.8%) of females with waist circumference equivalent or above 80 cm. 382(64.9%) had a systolic blood pressure equivalent or above 130 mmHg.
The overall macronutrient intake means were 1800.9(1434.9), 229.3(157.5), 80.5 (37), and 53.5(69.1), for calories, carbohydrates, protein, and fat, respectively. The metabolic equivalent was 112.3(425) min/week reflecting average energy expenditure in patients with diabetes following up in primary care facilities.
Regarding stages of behavior change, 214(36.3%) participants are in contemplation phase, 135(22.9%) in action, 96(16.3%) preparation, 69(11.7%) maintaining current healthy behavior, 49 (8.3%) at pre-contemplation, and 26(4.4%) relapsed. Surprisingly, 175(~ 30%) of participants did not declare any barriers to behavior change.
Comparing intervention with control
Socio-demographic: 153(53.7%) of participants were females in intervention group versus 195(64.1%) in control. Median age was 46(IQR=52-41) and 49(IQR=56–42) in intervention and control group, respectively. Participants aged between 35 and 59 years old made 225(78.9%) and 242(79.6%), in intervention and control, respectively.
Outcome of Interest
Mean difference in glycemic parameters
Table 1 shows the means, medians, and p-values of the glycemic indicators in patients with diabetes in intervention versus control. There was no marked difference in mean weight, BMI, LDL-C, or HDL-C between the two groups. The same with median waist circumference, HbA1c, systolic and diastolic blood pressure, no strong evidence to support a big difference in both intervention and control groups (Table 1).
| Overall result | Intervention | Control | Mean/median difference (95% CI) | p-value | |
|---|---|---|---|---|---|
| Participants N (%) | 589(100%) | 285(48.4%) | 304(51.6%) | … | … |
| 241(40.9%) | 132(46.3%) | 109(35.9%) | … | … | |
| Males N (%) | |||||
| Females N (%) | 348(59.1%) | 153(53.7%) | 195(64.1%) | … | … |
| Median age (IQR) years old | 47(55-41) | 46(52-41) | 49(56-42) | … | … |
| Young adults (18 to 34.9 years old) N (%) | 55(9.3%) | 32(58.2%) | 23(41.8%) | ||
| Middle age (35 to 59.9 years old) N (%) | 467(79.3%) | 225(48.2%) | 242(51.8%) | ||
| Elderly (60 years old and above) N (%) | 67(11.4%) | 28(41.8%) | 39(58.2%) | ||
| Mean weight (SD) Kg | 83.6(47.2) | 82.6(17.5) | 84.5(17) | -2.0(-4.75 to 0.83) | 0.92 |
| Mean BMI (SD) kg/m2 | 33(9.9) | 31.2(7.3) | 34.7(11.5) | -3.5(-5.0 to 1.8) | 1 |
| Mean waist circumference (SD) cm | 105.1(13.1) | 102(13.2) | 107(12.7) | -4.2(-6.3 to 2.1) | 1 |
| Mean HbA1c (SD)% | 7.8(1.9) | 7.6(1.9) | 8.0(1.8) | -0.44(-0.75 to 0.14) | 0.99 |
| Median systolic blood pressure (IQR) mmHg | 134(149-124) | 133(145-124) | 137(150-125) | … | 0.125 |
| Median diastolic blood pressure (IQR) | 80(88-72) | 80(86-70) | 80(90-74) | … | 0.162 |
| Mean LDL-C (SD) g/dl | 2.9(0.9) | 2.9(0.9) | 2.8(0.9) | 0.1(-0.2 to 0.1) | 0.771 |
| Mean HDL-C (SD) | 1.2(0.4) | 1.2(0.3) | 1.2(0.4) | -0.01 (-0.07 to 0.04) | 0.683 |
Table 1: Summary statistics of baseline clinical & glycemic parameters for patients with diabetes in control vs. intervention group. N(%): Number (percentage); 95% CI: Confidence Interval; IQR: Inter Quartile Range; SD: Standard Deviation.
Table 2 presents the frequency of patients who achieved the target values for glycemic control in intervention and control group. 122(56.5%) vs. 94(43.5%) for glycated hemoglobin less than 7, 33 (55.9%) vs. 26 (44.1%) for LDL-cholesterol less than 1.8, 63(50%) vs. 63(50%) for HDL-cholesterol, 153(42.6%) vs. 206(57.4%) for BMI>=30, 176(46.1%) vs. 206(53.9%) for systolic and 109(52.7%) vs. 98(47.3%) for diastolic blood pressure (Table 2).
| Overall result | Intervention | Control | p-value | |
|---|---|---|---|---|
| HbA1c>=7 | 373(63.3%) | 163(43.7%) | 210(56.3%) | 0.033 |
| HbA1c<7 | 216(36.7%) | 122(56.5%) | 94(43.5%) | |
| LDL-C>=1.8 | 530(90%) | 252(47.6%) | 278(52.5%) | 0.223 |
| LDL-C<1.8 | 59(10%) | 33(55.9%) | 26(44.1%) | |
| HDL -C>=1 | 463(78.6%) | 222(48%) | 241(52%) | 0.683 |
| HDL-C<1 | 126(21.4) | 63(50%) | 63(50%) | |
| BMI >=30 | 359(61%) | 153(42.6%) | 206(57.4%) | 0 |
| BMI 25 to 29.9 | 179(30.4%) | 94(52.5%) | 85(47.5%) | |
| BMI 18.5 to 24.9 | 51(8.7%) | 38(74.5%) | 13(25.5%) | 0.746 |
| WC>=94 in male | 214(36.3%) | 118(55.1%) | 96(44.9%) | |
| WC<94 in male | 27(4.6%) | 14(51.9%) | 13(48.2%) | 0.364 |
| WC>=80 in females | 337(96.8%) | 147(43.6%) | 190(56.4%) | |
| WC<80 cm in females. | 11(3.2%) | 6(54.6%) | 5(45.5%) | |
| Systolic blood pressure>=130 mmHg | 382(64.9%) | 176(46.1%) | 206(53.9%) | 0.127 |
| Systolic blood pressure<130 mmHg | 207(35.1%) | 109(52.7%) | 98(47.3%) | |
| Total | 589(100%) | 285(48.4%) | 304(51.6%) |
Table 2: Comparing the frequency (percentage) of patients in intervention and control groups in relation to glycemic parameter goal target achievement.*According to the national guidelines for diabetes management. HbA1c=glycated hemoglobin; LDL-C: Low Density Lipoprotein Cholesterol; HDL-C: High Density Lipoprotein Cholesterol; BMI: Body Mass Index; WC: Waist Circumference.
Mean difference in macronutrient intake
Table 3 shows the means and (standard deviation) for calories, carbohydrates, protein, and fat in intervention and control groups. Difference in mean calories was 219.8 lower in the intervention compared with the control, with 95% CI -451.7 to 12.1. For other nutrients, including carbohydrates, protein, and fat, the difference in mean values were -11.9, -13.2 and -17.3 respectively, in intervention group compared with the control. However, 95% CI were -37.4 to 13.6, -19.1 to 7.3 and -28.4 to 6.2 for mean difference carbohydrates, protein, and fat, respectively.
Mean difference in energy expenditure
This was measured by calculating the mean MET (min/week) in participants using the GPAQ which was 68.6(47.8) in the intervention and 153.2(587.8) in the control with a mean difference of -84.7. However, the 95% CI was -153.3 to 16.1 and a p-value of 0.992 (Table 3).
| Overall result | Intervention | Control | Mean difference (95% CI) | p-value | |
|---|---|---|---|---|---|
| Mean calories (SD) | 1800.9 (1434.9) | 1687.4 (1633.3) | 1907.2 (1213.1) | -219.8(-451.7 to 12.1) | 0.968 |
| Mean carbs (SD) | 229.3 (157.5) | 223.1 (213) | 235 (74) | -11.9(37.4 to 13.6) | 0.819 |
| Mean protein (SD) | 80.5 (37) | 73.6 (37.7) | 86.9 (35.4) | -13.2(-19.1 to 7.3) | 0.427 |
| Mean fat (SD) | 53.5 (69.1) | 44.6 (26.3) | 61.8 (92) | -17.3(-28.4 to 6.2) | 0.998 |
| Mean MET-minutes/ week (SD) | 112.3 (425.4) | 68.6 (47.8) | 153.2 (587.8) | -84.7(-153.3 to 16.1) | 0.992 |
| Steps /week*** | 0 | 0 | 0 | … | … |
Table 3: Summary statistics of dietary intake* and physical activity** parameters for patients with diabetes, comparing control vs. intervention group. *Assessment of dietary intake within 24 hours using FFQ tool. **Assessment of physical activity within the last 7 days using GPAQ. ***pedometer bands were used steps count. 95% CI: Confidence Interval; SD: Standard Deviation; MET: Metabolic Equivalent.
Frequency of patients according to stages of behavior change
Majority of participants in intervention were in the contemplation phase, 150(52.6%), while the majority of the control were in action stage, 94(30.9%). Table 4 shows the frequency of patients in each stage of behavior change, in both groups with no strong evidence of difference between the two groups, p-value < 0.05 (Table 4).
| Stages of behavior change | Overall result | Intervention | Control | P-value |
|---|---|---|---|---|
| Precontemplation | 49(8.3%) | 3(6.1%) | 46(93.9%) | |
| Contemplation | 214(36.3%) | 150(70.1%) | 64(29.9%) | |
| Preparation | 96(16.3%) | 35(36.5%) | 61(63.5%) | 0.127 |
| action | 135(22.9%) | 41(30.4%) | 94(69.6%) | |
| Maintenance | 69(11.7%) | 45(65.2%) | 24(34.8%) | |
| Relapse | 26(4.4%) | 11(42.3%) | 15(57.7%) | |
| Total | 589(100%) | 285(48.4%) | 304(51.6%) |
Table 4: Comparing the frequency (percentage) of patients in relation to the stages of behavior change.
Frequency of patients according to reasons against behavior change
In the intervention group, the most common reason that interferes with behavior change was lack of knowledge; 65(22.8%). However, 63(22.1%) find no reasons that might hinder their willingness to behavior change. In the control group, 112(36.8%) patients did not have any reason for halting behavior change, the most frequent answer. Similar to difference in patients’ frequency in relation to stages of behavior change, p-values were <0.05 (Table 5).
| Barriers for behavior change | Overall result | Intervention | Control | P-value |
|---|---|---|---|---|
| No reason | 175(29.7%) | 63(36%) | 112(64%) | |
| Fear from failure | 9(1.5%) | 6(66.7%) | 3(33.3% | |
| Fear from change | 9(1.5%) | 3(33.3%) | 6(66.7%) | |
| Lack of time | 111(18.9%) | 54(48.7%) | 57(51.3%) | |
| Lack of support | 6(1.0%) | 3(50%) | 3(50%) | |
| Lack of knowledge | 94(16.0%) | 65(69.2%) | 29(30.9%) | 0.562 |
| Lack of motivation | 100(17%) | 57(57%) | 43(43%) | |
| Limited access to health care | 9(1.5%) | 4(44.4%) | 5(55.6%) | |
| Peer pressure | 14(2.4%) | 8(57.1%) | 6(42.9%) | |
| Stress | 57(9.7%) | 18(31.6%) | 39(68.4%) | |
| Socioeconomic factor | 4(0.7%) | 4(100%) | 0 | |
| Limited access to food | 1(0.2 %) | 0 | 1(100%) | |
| Total | 589(100%) | 285(48.4%) | 304(51.6%) |
Table 5: Comparing the frequency (percentage) of patients in relation to barriers for behavior change
Discussion
This is a post hoc analysis of baseline data of an ongoing trial, aiming at describing the general characteristics of study population and measuring the comparability of the intervention group (multi-modality intervention) in comparison with the control (usual care), at baseline phase.
Out of 700 participants who verbally acknowledged their desire to be part of the trial, 589 participants provided an informed consent and were randomized into intervention and control groups: 285(48.4%) in the intervention arm and 304 (51.6%) in the control.
The impact of COVID-19 pandemic on clinical trials and research studies have been significant [18-20]. Most research projects other than COVID-19 are experiencing a delay in timelines and a substantial halt of operations, thus affecting clinical research progress and outcomes. In the field of cardiovascular disease management, 892 trials evaluating the efficacy of a range of treatments were kept on hold during the pandemic. The UK national institute of health research reported that many trials had to withhold the recruitment phase due to lack of site research staff and government restrictions that mandates minimizing face to face contact with patients unless urgently required.
Overall, the study showed that majority of participants were females 348(59.1%) and of middle age. The average body mass index was 33 kg/m2 indicating high prevalence of obesity among patients with diabetes. In addition, central obesity was prominent in women where more than 90% had waist circumference of >=80 cm, with an average waist circumference of 105.1. The mean for glycated hemoglobin was 7.8% and above 60% of participants have had a glycated hemoglobin level of more than 721 However, that level of glycated hemoglobin is not always the cut-off value that determines bad control, in fact it depends on patients’ age and presence of comorbidity [21-22].
Dyslipidemia was prevalent in this study where 90% of participants have had an LDL-C of more than 1.8 mg/dl and average LDL-cholesterol of 2.9 g/dl. According to lipid goal guidelines of diabetes management, LDL-C<1.8 mg/dl is required to prevent recurrent cardiovascular events in patients with diabetes [23-25].
Optimal systolic blood pressure was achieved by 35% of diabetes population, with large proportion of patients have beyond the target level for blood pressure that is required to avoid serious [26,27].
In terms of sociodemographic comparability, both intervention and control had larger proportion of females compared to males and middle age population compared to other age groups.
The overall glycemic parameters were lower in the intervention arm, where average HbA1c, BMI, waist circumference, systolic and diastolic blood pressure, and HDL- cholesterol were lower in the intervention compared to the control. However, the size of difference was insignificant, and evidence did not support the presence of this difference. The same was noticed in macronutrient intake and energy expenditure, where the means for calories, carbohydrate, protein, fat and MET was lower in the intervention arm. The amount of difference was small and evidence to support this different was weak. Thus, the compatibility of both arm in regards of glycemic indicators, macronutrient consumption, and physical activity is ensured.
Based on our result on behavior change, majority of patients in intervention arm reported having awareness and understanding of how important it is to improve their current lifestyle but are not yet ready for change. In contrary to that, most participants in the control arm are in the action stage where patients are following a healthy lifestyle regime to achieve glycemic control. The most common barriers to change in the intervention was lack of knowledge, followed by no reason, lack of motivation, and lack of time. In the control, no reason was reported the most, followed by lack of time, lack of motivation, and stress. Generally, willingness and barriers to behavior change were measured subjectively during baseline counselling, where risk of information bias is possible and overestimated reports are expected.
The limitation of our study is the high dropout rate during the recruitment phase was a challenge, but it did not exceed 20%. Information bias is possible in assessing lifestyle style as subjective methods are used in measuring that. The strength is found in adopting the pre-existing guidelines on conducting clinical trials during COVID-19 pandemic, that strengths trial’s methodology and ensuring the feasibility of participation.
We will use remote monitoring and follow up during the next phases throughout 12 months period, until endpoint assessment is achieved, probably in January 2023. Several health centers were enrolled in this study to ensure the heterogeneity of patients with diabetes hence generalizability of study result.
Despite the challenges faced on recruitment amid COVID-19 pandemic, more than 80% of the target participants were enrolled. The trial managed to Overall, there is no evidence of a difference in baseline characteristics including socio-demographic, glycemic parameters, willingness for behavior change, nutritional and physical activity status, hence the two groups are similar.
Conclusion
The trial’s population at baseline were comparable in terms of demographic and clinical characteristic, minimizing the risk of selection bias in this interventional study.
Acknowledgment
We thank the director of primary care, Dr Huda Anwar in supporting the flow of this trial in the health centers; the in charges of health center at A’Seeb district health for facilitating the flow of this trial; All clinicians and nurses who participated in blood sample collection and vital sign measurement. Lastly, we would like to express our special thanks to all participating patients from A’Seeb district health centers for their time and support.
Declaration of Conflicting Interests
The authors declare that there is no conflict of interest.
Refernces
- Ogurtsova K, da Rocha Fernandes JD, Huang Y, Linnenkamp U, Guariguata L, et al. (2017) IDF diabetes atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract 128: 40-50.
[Crossref], [Google Scholar], [Indexed] - Entmacher PS, Marks HH (1965) Diabetes in 1964: A world survey. Diabetes 14: 212-23.
[Crossref], [Google Scholar], [Indexed] - Rathmann W, Giani G (2004) Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care 27: 2568-9.
[Crossref], [Google Scholar], [Indexed] - Whiting DR, Guariguata L, Weil C, Shaw J (2011) IDF diabetes atlas: Global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 94: 311-21.
[Crossref], [Google Scholar], [Indexed] - Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, et al. (2021) IDF diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract 2021: 109119.
[Crossref], [Google Scholar], [Indexed] - Al-Mawali A, Al-Harrasi A, Jayapal SK, Morsi M, Pinto AD, et al. (2021) Prevalence and risk factors of diabetes in a large community-based study in the Sultanate of Oman: STEPS survey 2017. BMC Endocr Disord 21: 42.
[Crossref], [Google Scholar], [Indexed] - Oman (2018) Global burden of disease study 2017.
- Guthold R, Stevens GA, Riley LM, Bull FC (2018) Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Health 6: e1077-e86.
[Crossref], [Google Scholar], [Indexed] - Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, et al. (2012) Sedentary time in adults and the association with diabetes, cardiovascular disease and death: Systematic review and meta-analysis. Diabetologia 55: 2895-905.
[Crossref], [Google Scholar], [Indexed] - Edwardson CL, Gorely T, Davies MJ, Gray LJ, Khunti K, et al. (2012) Association of sedentary behaviour with metabolic syndrome: A meta-analysis. PLoS One 7: e34916.
[Crossref], [Google Scholar], [Indexed] - Bell JA, Hamer M, Batty GD, Singh-Manoux A, Sabia S, et al. (2014) Combined effect of physical activity and leisure time sitting on long-term risk of incident obesity and metabolic risk factor clustering. Diabetologia 57: 2048-56.
[Crossref], [Google Scholar], [Indexed] - Doehner W, Gerstein HC, Ried J, Jung H, Asbrand C, et al. (2020) Obesity and weight loss are inversely related to mortality and cardiovascular outcome in prediabetes and type 2 diabetes: Data from the ORIGIN trial. Eur Heart J 41: 2668-77.
[Crossref], [Google Scholar] - Liu X, Ju W, Huo C, Zhang S, Wang X, et al. (2021) Overweight and obesity as independent factors for increased risk of hepatocellular cancer-related mortality: A Meta-Analysis. J Am Coll Nutr 40: 287-93. [Crossref], [Google Scholar], [Indexed]
- Okunogbe A, Nugent R, Spencer G, Ralston J, Wilding J (2021) Economic impacts of overweight and obesity: Current and future estimates for eight countries. BMJ Glob Health 6.
[Crossref], [Google Scholar], [Indexed] - Yousif JH, Khan FR, Zia K, Saadi NA (2021) Analytical data review to determine the factors impacting risk of diabetes in North Al-Batinah region, Oman. Int J Environ Res Public Health 18.
[Crossref], [Google Scholar], [Indexed] - Al Ghafri T, Anwar H, Al Hinai E, Al Harthi T, Al Jufaili F, et al. (2021) Study protocol: Behaviour change intervention to promote healthy diet and physical activity in overweight/obese adults with diabetes attending health care facilities in Muscat: A cluster rendomised control trial. BMC Public Health 21: 1529.
[Crossref], [Google Scholar], [Indexed] - Lorette G, Maruani A (2013) (The CONSORT statement (CONsolidated standards of reporting trials)). Ann Dermatol Venereol 140: 431-5.
[Crossref], [Google Scholar], [Indexed] - Sathian B, Asim M, Banerjee I, Pizarro AB, Roy B, et al. (2020) Impact of COVID-19 on clinical trials and clinical research: A systematic review. Nepal J Epidemiol 10: 878.
[Crossref], [Google Scholar], [Indexed] - Gaba P, Bhatt DL (2020) The COVID-19 pandemic: A catalyst to improve clinical trials. Nat Rev Cardiol 17: 673-5.
[Crossref], [Google Scholar], [Indexed] - Mitchell EJ, Ahmed K, Breeman S, Cotton S, Constable L, et al. (2020) It is unprecedented: Trial management during the COVID-19 pandemic and beyond. Trials 21: 1-7.
[Crossref], [Google Scholar] - Gavi S, Hensley J (2009) Diagnosis and management of type 2 diabetes in adults: A review of the ICSI guideline. Geriatrics 64: 12-7.
[Crossref], [Google Scholar], [Indexed] - Guideline development group (2015) Clinical practice guideline on management of patients with diabetes and chronic kidney disease stage 3b or higher (eGFR <45 mL/min). Nephrol Dial Transplant 30: ii1-142.
[Crossref], [Google Scholar], [Indexed] - Ferrieres J, Lautsch D, Bramlage P, Horack M, Baxter CA, et al. (2020) Lipid-lowering treatment and low-density lipoprotein cholesterol target achievement in patients with type 2 diabetes and acute coronary syndrome. Arch Cardiovasc Dis 113: 617-29.
[Crossref], [Google Scholar], [Indexed] - Malek F, Dvorak IJ, Strieborna H, Kocvarova V, Spacek R (2008) Reaching target lipid levels and the natural history of diabetes mellitus in patients surviving acute coronary syndrome: A retrospective cohort study from a tertiary care outpatient clinic. Exp Clin Cardiol 13: 25-8.
[Crossref], [Google Scholar], [Indexed] - Beard AJ, Hofer TP, Downs JR, Lucatorto M, Klamerus ML, et al. (2013) Assessing appropriateness of lipid management among patients with diabetes mellitus: Moving from target to treatment. Circ Cardiovasc Qual Outcomes 6: 66-74.
[Crossref], [Google Scholar], [Indexed] - Kjeldsen SE, Mariampillai JE, Nilsson PM (2018) Optimal blood pressure target in diabetic and nondiabetic hypertensive patients. Circ Res 123: 528-30.
[Crossref], [Google Scholar], [Indexed] - Group AS, Cushman WC, Evans GW, Byington RP, Goff DC, et al. (2010) Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 362: 1575-85.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences