Care Guidance Supports Health Systems and Mental Health Providers with Advancing Behavioral Health Equity, Avoiding Relapses and Readmissions
Craig Parker
Department of Behavioral Health Equity, Guideway Care, Birmingham, USA
Published Date: 2023-10-23DOIDOI: 10.36648/2572-5483.8.5.215
Craig Parker1* and Heather Ridenoure2
1Department of Behavioral Health Equity, Guideway Care, Birmingham, USA
2Department of Healthcare Strategy, Contigo Health, Charlotte, USA
- *Corresponding Author:
- Craig Parker
Department of Behavioral Health Equity,
Guideway Care, Birmingham,
USA,
E-mail: craig.parker@guidewaycare.com; ejin@cpronline.com
Received date: September 21, 2023, Manuscript No. IPJPM-23-17914; Editor assigned date: September 25, 2023, PreQC No. IPJPM-23-17914 (PQ); Reviewed date: October 09, 2023, QC No. IPJPM-23-17914; Revised date: October 16, 2023, Manuscript No. IPJPM-23-17914 (R); Published date: October 23, 2023, DOI: 10.36648/2572-5483.8.5.215
Citation: Parker C, Ridenoure H (2023) Care Guidance Supports Health Systems and Mental Health Providers with Advancing Behavioral Health Equity Avoiding Relapses and Readmissions. J Prev Med Vol.8 No.5:215.
Abstract
Americans are struggling at home and in the workplace with mental and behavioral health conditions as a national surge in post-COVID demand persists for psychiatric care, substance use disorder treatment and clinical counseling. In many circumstances, there remain unmet care needs and avoidable barriers to accessing mental and behavioral health services to address residual stress, anxiety, substance use and depression. Additionally, the impact of Social Determinants of Health (SDoH) the non-clinical, socioeconomic factors that widen disparities and pose barriers to accessing quality care, affect health outcomes, increase risks of relapses and readmissions compounds the behavioral health crisis from both patient and provider perspectives. Addressing the SDoH issues that underlie a number of disparities among at risk patients is key to advancing behavioral health equity. This approach works to remove previously unrecognized barriers to care and to open up a patient’s ability to receive quality mental and behavioral health services. It further supports continuation of care and treatment adherence for those with one or more co-occurring conditions, while fostering preventive efforts by proactively resolving non-clinical issues before they become clinically problematic.
Keywords
Behavioral health equity; Social determinants of health; Health disparities; Value-based care; Avoidable hospital readmissions; Care guidance; National nurse shortage; Patient activation
Key Points
• Recognizing and addressing Social Determinants of Health (SDoH) that disproportionately affect certain communities is crucial for promoting equity in behavioral health.
• Focusing on prevention and early intervention efforts can help identify and address behavioral health issues before they become more severe, reducing disparities in health outcomes.
• Improving data collection and analysis practices can help identify disparities and assess the effectiveness of interventions in different populations.
• Collaboration with a care guidance provider who can support a patient with non-clinical needs is essential to create a coordinated approach to address behavioral health equity.
Introduction
Ensuring access to mental and behavioral health services to all who are in crisis or at-risk is one of the most challenging priorities in healthcare today. In fact, providing for the estimated 43.8 million Americans [1] who experience mental illness is so critical that President Biden declared it a national mental health crisis during his 2022 State of the Union address [2]. Just as important to the clinical response of mental and behavioral health emergencies is the prevention of avoidable conditions rooted in non-clinical factors and that diminish behavioral health equity, defined as the right of all individuals, regardless of race, age, ethnicity, gender, disability, socioeconomic status, sexual orientation, or geographical location, to access high-quality and affordable healthcare services and support [3]. Successful prevention involves employing dedicated and focused resources and applying strategic interventions that work to recognize and resolve at-risk patient issues along the continuum of care to prevent mental, behavioral and physical health deteriorations that would require costly utilization of clinical services. A surge in demand for clinical psychiatric care to treat acute mental and behavioral health conditions severely strains hospital resources and provider staff and reveals the vulnerabilities of the healthcare system. Due to the fragmented nature of the healthcare infrastructure, persistent lack of sufficient resources and longstanding shortages of mental and behavioral health professionals, far too many Americans have limited access to the professional, personalized and preventive care they need and deserve.
Material and Methods
Behavioral health inequities widen disparities
Healthcare providers must consider the full spectrum of needs and circumstances of each individual patient and recognize the demographics and related non-clinical issues underlie health inequities and can compound their mental and behavioral health condition(s). In fact, non-clinical issues contribute 80% to 90% of the modifiable contributors to a patient’s well-being [4].
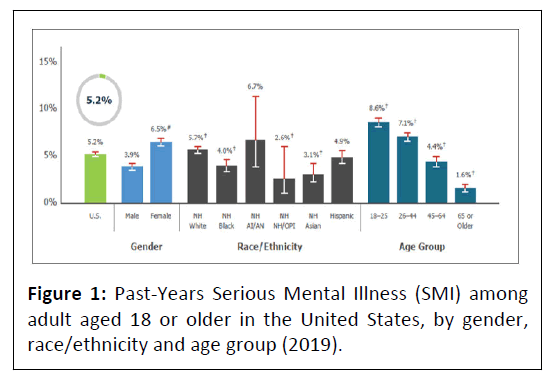
To identify populations most at risk, the Substance Abuse and Mental Health Services Administration’s (SAMSHA) Behavioral Health Equity Report 2021 disaggregates behavioral health indicators by selected factors, including race and ethnicity, income level, county type, and health insurance status [5] (Figure 1).
Source: SAMSHA. As per the source https://www.samhsa.gov/behavioral-health-equity, within the spectrum of non-clinical factors are Social Determinants of Health (SDoH) [6]. These include housing, food and nutrition, transportation, social and economic mobility, education and environmental conditions. These aspects of SDoH influence heath disparities, defined as the preventable differences in the burden of disease or opportunities to achieve optimal health that are experienced by socially disadvantaged patient populations [7].
Strategy: Identify and resolve non-clinical issues that pose barriers to care
Recognizing and addressing SDoH that disproportionately affect certain communities is crucial for promoting behavioral health equity. In the context of mental health, disparities challenge patients by creating barriers to accessing and adhering to their care, especially when and where care is critically needed. Focusing on prevention and early intervention efforts can help identify and address behavioral health issues before they become more severe. If SDoH issues and their potential barriers to care are not promptly resolved, they can lead to further health deteriorations, extended hospitalizations and avoidable readmissions that require costly utilization of clinical services. As many behavioral and mental health conditions are chronic, this utilization and unmet care needs can lead to a significant trend increase over a patient’s lifetime. For example, one systematic review synthesized risk factors associated with 30-days unplanned hospital readmissions for patients with mental illness and consistently cited as readmission predictors patients with lower educational background, unemployment, previous mental illness hospital admission and more than 7 days of the index hospitalization [8]. As SDoH exist at the individual patient level and within communities, they typically fall outside of the health system’s visibility and control. Patients who are at risk of SDoH-driven disparities typically require an amplified level of personalized support with higher levels of activation and monitoring beyond the provider’s focus on clinical care. This is especially true with patient transitions from the hospital or care facility to home-based care.
Solution: Care guidance
Given the importance of resolving non-clinical issues and barriers and advancing health equity among at-risk patient populations, health system administrators are looking for innovative, yet cost-effective solutions. However, given that national staffing shortages are the new normal in healthcare, many organizations are finding it difficult to find the right kind and enough of the professional Care Guides to build sustainable and effective interaction models. To support an equitable path forward for behavioral health patients, health systems are employing patient advocates whose scope is focused on communicating with and activating patients to proactively identify and promptly and resolve their health disparities before they manifest and become problematic and costly [9]. The integral role of care guidance, also referred to as “care navigation,” serves as an extension of a hospital’s clinical team to support a range of care management activities, including facilitating pre-and-post-discharge, identifying non-clinical and community support resources and promoting continuation of care.
How care guidance works
The primary goal of care guidance is to ensure that the patient receives the right care at the right time, in the right place and with the right outcome. Keeping a patient on track is accomplished through specially selected and tech-enabled “Care Guides” who work to establish a peer-to-patient connection with patients and their families. This human-led approach builds trust, lowers a patient’s resistance to sharing information and helps to uncover potential barriers they encounter. Optimally, Care Guides are equipped with scalable, technology platforms that provide structured workflows and use evidence-based disease and condition-specific protocols to proactively identify and resolve non-clinical barriers while also using standard symptom assessments. Through this level of support, Care Guides ensure that patients are enrolled in the most applicable and supportive programs and can make sure patients are taking advantage of their Annual Wellness Visit (AWV) and other health system and community benefits. Moreover, when Care Guides are engaged with patients, clinical issues can be found and immediately escalated to proper clinical care teams. The human element of care guidance is especially important as digital engagement simply cannot be a replacement for the human aspect of patient interaction. This is especially true considering the limited abilities certain populations have in accessing digital technologies, and potential use impairments among disabled, disadvantaged and senior populations. Human and tech elements, integrated together, are effective in identifying practical issues and enabling proactive resolution of non-clinical barriers to a patient’s continuum of care.
Results
A successful care guidance program renders a Return on Investment (ROI) through improved efficiencies, reduced time and resource allocation and cost of over utilizing clinical care teams. Care guidance is of especially high value in alleviating non-clinical tasks and its support of navigating patients through the complexities of the healthcare system, especially when patients have co-occurring mental and behavioral health disorders (e.g., substance use disorder and anxiety). For example, helping patients understand their discharge instructions, scheduling follow-up appointments, supporting medication fulfilment and compliance and ensuring needed transportation highlight the importance of connected care and patient activation.
Behavioral health success stories
Following are “success stories” of behavioral health patients who experienced clinical issues including anxiety and depression and who benefitted from care guidance in support of resolving non-clinical barriers to their continuum of care, as well as being credited for improvements in their patient experience and quality of life.
Cooper Green Mercy Health Services, an affiliate of the UAB Health System, provides high-quality health care to all residents of Jefferson County, regardless of ability to pay. It is a full-service ambulatory care facility that includes primary and specialty care clinics; urgent care; physical, occupational and speech therapy; laboratory services; imaging; and pharmacy, all conveniently available to patients in one location.
• “The Care Guide contacted the patient for outreach and several assessments. The patient expressed the need for help with several appointments. The Care Guide was able to reach out to Yolanda for help making a behavioral health appointment; she was also able to connect with the patient's PCP to request referral for dental appointment. After several calls, the Care Guide confirmed dental appointments for the patient and the patient thanked her for all the help.”
• “The patient advised that the Care Guide has made such a difference in her life and if the Care Guide hadn't been there to call her, she didn't know what would've happened. She said that the Care Guide has been so kind, patient and caring towards her. The Care Guide has made a difference in her life for the better, and she's very grateful for this service.”
• “The patient wanted to thank the Care Guide for all her help. He now has a job (the Care Guide referred him to a job center), is working on buying a house and advised he is happier and sleeps better since she initiated contact. The patient stated he wanted to "reward her" with free dinner but the Care Guide advised the patient the best reward was seeing him succeed. The patient was very thankful and grateful for the help and continued support.”
• “The patient was so thankful for all the help the Care Guide has given her. She stated she wouldn't have known where to start (solving her issues). The patient stated that the Care Guide is always kind and helpful and she is so thankful.”
• “The patient advised that she is thankful for the Care Guidance program and having the Care Guide to help her. She stated before the Care Guide started calling her, she felt lost, and it was all on her to figure it out. But since starting the program she has felt so cared about and informed. Patient thanked the Care Guide for all the help and is so grateful.”
Patient stories
The following real-life patient stories demonstrate the value of care guidance. In these cases, the patients were able to avoid emergency room or hospitalization and did not require rehabilitation.
• The patient advised that the Care Guide has made such a difference in her life and if the Care Guide hadn't been there to call her, she didn't know what would've happened. She said that the Care Guide has been so kind, patient and caring towards her. The Care Guide has made a difference in her life for the better, and she's very grateful for this service. Primary issue: Anxiety; Age: 56 y/o Female.
• The patient wanted to thank the Care Guide for all her help. He now has a job (the Care Guide referred him to a job center), is working on buying a house and advised he is happier and sleeps better since she initiated contact. The patient stated he wanted to "reward her" with free dinner but the Care Guide advised the patient the best reward was seeing him succeed. The patient was very thankful and grateful for the help and continued support. Primary issue: Anxiety; Age: 34 y/o Male.
• The patient was so thankful for all the help the Care Guide has given her. She stated she wouldn't have known where to start (solving her issues). The patient stated that the Care Guide is always kind and helpful and she is so thankful. Primary issue: Bipolar; Age: 51 y/o Female.
• The patient advised that she is thankful for the Care Guidance program and having the Care Guide to help her. She stated before the Care Guide started calling her, she felt lost, and it was all on her to figure it out. But since starting the program she has felt so cared about and informed. Patient thanked the Care Guide for all the help and is so grateful. Primary issue: Anxiety; Age: 56 y/o Female.
Propositions of a care guidance program
Data captures SDOH insights: Improving data collection and analysis practices can help identify disparities and assess the effectiveness of interventions in different populations. An effective care guidance program captures SDoH data and disparity-related barrier resolution for operational improvement. This data can supplement the capabilities of Electronic Medical Records (EHR) systems. AI and machine learning can be applied to anticipate patient needs based upon condition-specific protocols that enable care guides to deliver an unprecedented level of vital, just-in-time communication. Led by this intelligence, care guides provide patients with the information they need to engage in the process of their care and empower each patient to receive a better understanding of their treatment plan and compliance options.
Ensures treatment adherence and medication compliance: Medication adherence among behavioral health patients are a complex issue determined by a multitude of factors, such as treatment effect, patient insight, attitudes toward medication, history of substance use, financial and emotional support from family members, income situation, side effects, cultural context, level of therapeutic alliance with therapists and aftercare environment after discharge. A clear understanding of the treatment plan can help with motivation to stay on track with the treatment plan which in turn drives better adherence and compliance with recommended [10]. Care guidance provides behavioral patients with personalized care navigation to increase medication compliance and treatment plan adherence, optimizing post-discharge medication adherence and avoiding adverse events.
Assists with scheduling and appointment reminders: The national average of missed patient appointments is 20% in behavioral health. Findings suggest that psychiatric prehospitalization is associated with discontinuity of contact with psychiatric services but not with diagnosis [11]. Recommended post-discharge treatment includes a visit with a mental health provider within 30 days after discharge. Ideally, patients should see a mental health provider within 7 days after discharge. Follow-up care after hospitalization for mental illness or intentional self-harm helps improve health outcomes and prevent readmissions [12]. With extended support that is proven to have positive and profound results for delivering personalized and preventive patient-centric care, care guidance provides an equitable path forward for behavioral health patients. Health systems and mental health treatment facilities are engaging in care guidance programs that employ patient advocates and navigators whose scope is activating patients to identify and promptly resolve their health disparities-before they become problematic and costly.
Aligns with priorities of value-based care: SDoH historically were not considered within the realm of public health or chronic disease prevention. However, driven by organizations like The Joint Commission, CMS’ framework for health equity and data from value-based care programs, hospital administrators and providers are quickly understanding their influence on clinical health [13,14]. Improving health equity is a quality and safety priority of The Joint Commission. Leading with its National Patient Safety Goals (NPSG) standards, the organization continues to elevate the importance of health equity as it impacts healthcare quality and outcomes [15]. The Joint Commission has taken a major step towards advancing health equity with the launch of a voluntary Health Equity Certification Program (HECP) [16]. Given Medicaid’s role in delivering care to low-income individuals, the program is uniquely situated to address related health disparities. Value-based payment, which many payers are already utilizing to encourage improved health outcomes and more efficient care, can be a strong tool to design equity-focused payment and contracting models (payment approaches). These equity-focused payment approaches can support and incentivize care delivery transformation to reduce and eliminate disparities in health and health care [17].
Discussion
Benefits of a care guidance partnership
Care guidance is rapidly becoming a “must-have” addition to the service portfolio of health systems, hospitals and provider organizations. It is at the nexus of new managed care priorities where care guidance represents an innovative approach to advancing health equity and delivering “high-value, high-quality care.” For hospital systems, partnerships can be effective options to sustain service lines and access to care in their communities [18]. This type of collaboration has increased significantly in the past decade, with hospitals and health systems looking to create operational, strategic and financial value to help them meet their mission of caring for patients and communities. For example, a hospital that does not offer a particular service line may seek a joint venture partnership with a leading organization in the field. These integrations not only preserve patient access to care, but they can also enhance quality of care. Attempting to allocate internal resources to perform the tasks that fall within the scope of care guides could potentially be both inefficient and costly. When an outsourced care guidance program is well designed, implemented and managed, it can provide a significant upside for the hospital, its clinical staff and patients. Through a care guidance partnership, clinical staff receive the extended support they need to ensure the delivery of equitable while collaborating with care guides to enhance patient experience, satisfaction and resumption of functioning, quality of life. This is where the proposition of a care guidance solution presents the most value for shareholders a validated approach to equitable and sustainable care. Partnering with hospitals, health systems, other providers, payers, employers and behavioral health treatment centers, care guidance positively impacts patient lives and drives financial and operational improvements. Effective collaboration between health care organizations, mental healthcare providers and care navigators supports a necessary triad of post-discharge care coordination and management, with care guides addressing, for example, treatment plan adherence, medication management and depression and anxiety screenings. A behavioral health partnership can help clinicians improve their quality of care. Providing integrated healthcare services allows for better tracking of patient progress and more efficient interventions.
Conclusion
A higher level of personalized and preventive care
Care guidance provides patients with a higher level of personalized and preventive care to improve the provider’s ability to deliver patient-centered care and generate the best possible health and wellness. Hospitals and their clinical staffs receive the extended support they need to advance health equity and deliver care that optimizes patient experience, satisfaction and generates the best possible outcomes. This is where the proposition of care guidance presents the most value to all shareholders.
About the Authors
Craig Parker, JD, CPA, CEO, Guideway Care, has spent most of the last twenty-five years operationalizing solutions that leverage technology and people to improve patient care and outcomes.
Heather Ridenoure, Vice President, Contigo Health, has more than twenty years of experience in various aspects of healthcare including the design of employer-purchased benefits, substance use disorder product design and strategy, quality/regulatory, project management, program operations, process improvement, benefit design, provision of clinical care, revenue cycle and electronic medical record.
References
- (2020) Mental health facts in America. National Institute of Mental Health. U.S. Department of Health and Human Services.
- (2022) President Biden to announce strategy to address our national mental health crisis, as part of unity agenda in his first state of the union. The White House.
- (2023) Behavioral health equity. Substance Abuse and Mental Health Services Administration (SAMHSA).
- Magnan S (2017) Social determinants of health 101 for health care: Five plus five. National Academy of Medicine, Washington, USA.
[Crossref]
- (2021) Behavioral health equity report 2021: Substance use and mental health indicators measured from the National Survey on Drug Use and Health (NSDUH), 2015–2019. Center for Behavioral Health Statistics and Quality.
- (2023) Social determinants of health. US Department of Health and Human Services.
- Ndugga N, Artiga S (2023) Disparities in health and health care: 5 key questions and answers. KFF.
- Zhou H, Ngune I, Albrecht MA, Della PR (2023) Risk factors associated with 30-days unplanned hospital readmission for patients with mental illness. Int J Ment Health Nurs 32: 30-53.
[Crossref], [Google scholar], [Indexed]
- Becker C, Zumbrunn S, Beck K, Vincent A, Loretz N, et al. (2021) Interventions to improve communication at hospital discharge and rates of readmission: A systematic review and meta-analysis. JAMA Netw Open 4: e2119346.
[Crossref], [Google scholar], [Indexed]
- Deng M, Zhai S, Ouyang X, Liu Z, Ross B (2022) Factors influencing medication adherence among patients with severe mental disorders from the perspective of mental health professionals. BMC Psychiatry 22: 22.
[Crossref], [Google scholar], [Indexed]
- Grinshpoon A, Lerner Y, Lurie TH, Zilber N, Ponizovsky AM (2021) Post-discharge contact with mental health clinics and psychiatric readmission: A 6-month follow-up study. Isr J Psychiatry Relat Sci 48: 262-267. [Crossref],
[Google scholar], [Indexed]
- Smith TE, Haselden M, Corbeil T, Wall MM, Tang F, et al. (2020) Effect of scheduling a post-discharge outpatient mental health appointment on the likelihood of successful transition from hospital to community-based care. J Clin Psychiatry 81: m13344.
[Crossref], [Google scholar], [Indexed]
- (2022) Advancing health care equity, together. The Joint Commission.
- McIver L (2022) The path forward: Improving data to advance health equity solutions. Centers for Medicare & Medicaid Services.
- (2022) The joint commission's national patient safety goals presentation for 2023. The Joint Commission.
- Bronk K (2023) The Joint Commission launches Health Care Equity Certification. The Joint Commission.
- Patel S, Smithey A, Tuck K, McGinnis T (2023) Leveraging value-based payment approaches to promote health equity: Key strategies for health care payers. AHE: 1-20.
- (2022) Rural hospital closures threaten access: Solutions to preserve care in local communities. American Hospital Association.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences