Demographic Profile Impacts HIV Testing Rates among Adolescents and Young Adults in South Bronx, NY
Mayer Sagy, Duke Nelson and Walid Michelen
DOI10.21767/2572-5483.100012
Mayer Sagy*, Duke Nelson and Walid Michelen
Morrisania Community Health Center, Gotham Health, NYC Health and Hospitals, Bronx, New York, USA
- *Corresponding Author:
- Mayer Sagy
Morrisania Community Health Center, Gotham Health
NYC Health and Hospitals, Bronx, New York, USA
Tel: 164-627-16425
E-mail: Mayer.Sagy@NYCHHC.org
Received date: May 04, 2017, Accepted date: June 19, 2017, Published date: June 27, 2017
Copyright: © 2017 Sagy M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
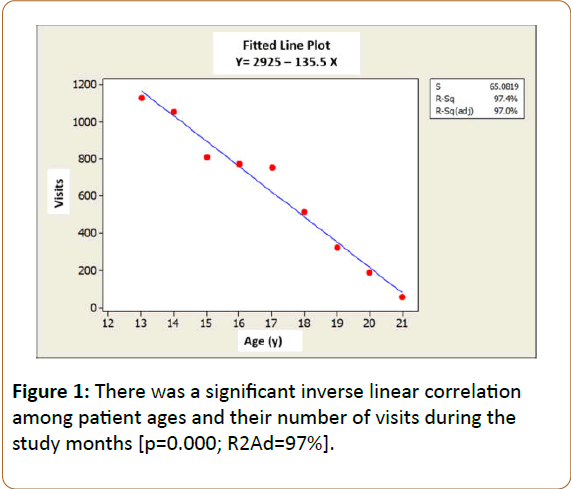
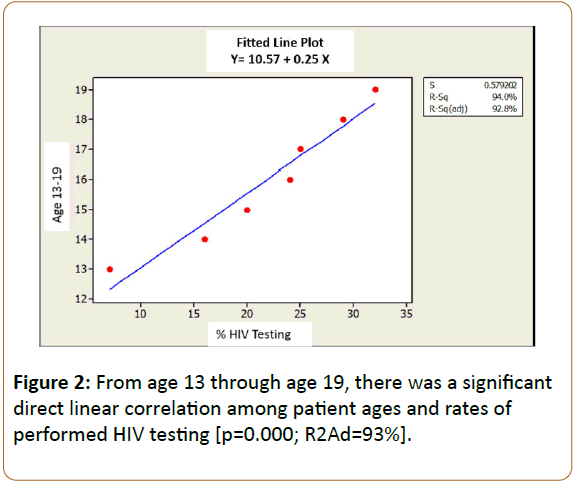
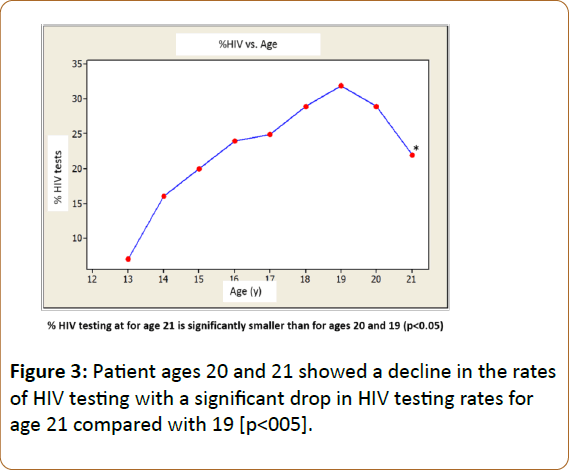
Introduction: Our Community Health Center offers routine HIV testing to all adolescents and young adults who are within the age range of 13 through 21 years. We sought to examine the effectiveness of our own program in relation to the demographic profile of the community we serve. Methods: Demographic datasets of 5,603 patient visits of adolescent patients and young adults who sought preventive care in our facility throughout a period of 16 months (years 2015-2016), were retrieved in an unidentified manner, tabulated and analyzed. Results: Only 3,775 (67%) patient visit charts included declared ethnicities while 1,586 [33%] did not. Out of the 3,775 declared races or ethnicities, the 3 main ones were, 2668 [71%] Hispanics, 978 (21%) blacks, 109 (3%) whites. The HIV testing rates in these 3 main ethnicities were 29% for whites, 20% for Hispanics and 18% for blacks [p<0.05 for whites compared to blacks and Hispanics]. There was a significant inverse linear correlation among patient ages and their number of clinic visits during the study period [p=0.000; R2Ad=97%]. From age 13 through age 19, there was a significant direct linear correlation among patient ages and rates of HIV testing [p=0.000; R2Ad=93%]. Patient ages of 20 and 21 years showed a decline in the rates of HIV testing. Conclusions: Compliance with HIV testing in South Bronx tends to be better among older teenagers and among patients of the white ethnicity. Compliance with scheduled clinic visits for preventive care declines as teenagers become older.
Keywords
HIV testing; Community; Infection; Adolescents
Introduction
HIV is an ongoing epidemic in the United States. While a significant progress in the treatment of affected patients has resulted in a significant improvement in their quality of life and in a longer life span, early detection of HIV infection continues to be a challenging undertaking for most healthcare centers [1]. In 2006, the US Centers for Disease Control and Prevention (CDC) recommended the implementation of a universal and routine HIV screening for all 13–64 year-olds regardless of their apparent risks for an HIV infection [2,3]. In 2011, the American Academy of Pediatrics (AAP) published a policy statement regarding routine HIV testing to adolescent and young adult patients indicating that routine screening should be offered, at least once, by 16 to 18 years of age when the prevalence of HIV in the patient population served is more than 0.1% [4]. Pediatricians have also been made aware of the fact that that an estimated 50% of patients who were proven to be infected with HIV had previously presented with pertinent HIV symptoms to their pediatric healthcare providers, yet, HIV was not considered in their differential diagnosis [5].
"Opt-out HIV testing” has been the current approach at our Community Healthcare Center in South Bronx. This approach refers to HIV testing being routinely offered and performed for all patients aged 13 to 21 years, unless the patients or their families decline [6]. This testing is offered whenever the patients arrive in the clinic for clinical preventive care visits and performed without a separate written informed consent or pretest counseling. However, issues of confidentiality and disclosure, particularly in adolescent care, make implementation of this initiative very challenging and therefore requires periodic assessment of the clinical benefits of such routine screening along with rates of patient compliance [7].
This study sought to evaluate our success rates in getting adolescents and young adults to agree to a quick HIV testing during their preventive care visits, and determine the impact of various demographic factors on such rates. We hypothesized that our documented rates of HIV testing among adolescents and young adult patients in South Bronx would be age and ethnicity related.
Material and Methods
Ethics
The study was conducted as a health center quality improvement project; it did not require an IRB approval for publication as it did not include any activities that involved “human subjects” according to published guidelines:(https://www.hhs.gov/ohrp/regulations-and-policy/guidance/faq/ quality-improvement-activities/index.html)
Methods
Patient documentation: All patients arriving in our facility were offered, as per policy, a rapid HIV antibody testing (OraQuick, Bethlehem, PA) by the patient care assistant (PCA). This was offered to all adolescents and young adults who were 13 to 21 years of age and who periodically sought preventive care visits. If the parent/patient agreed, the test was performed immediately after obtaining the patients’ vital signs. The performed HIV test was then noted in the patient’s electronic medical record (EMR); disagreements to HIV testing were also entered in the EMR with specific reasons for opting out. The policy also mandated that the HIV testing should be offered repeatedly to the same patients during each and every visit regardless of the fact that the tests may have been previously performed and regardless of previous notations of opting out.
Datasets retrieval: Data of all patients, aged 13-21 years, who had preventive care encounters with their primary care providers (PCP) at our facility, over a 16-month period, were retrospectively evaluated for demographic attributes. All demographic datasets were retrieved from the facility’s data warehouse that supported the software for patients’ registration entries (Soarian-Siemens Medical Solutions USA, Inc., Malvern, PA) and the medical information entries in their EMR (Quadramed-QuadraMed Corporation, Herndon, VA), by employing a business intelligence tool (Oracle BI Discover-Oracle Corporation, Redwood Shores, CA). These datasets were retrieved and tabulated in a de-identified manner to only include information regarding gender, age, ethnicity (race) and whether or not HIV testing was performed. Results of HIV testing were not retrieved for this quality performance evaluation.
Data analysis: Categorical data were analyzed by the Chi Square test for determination of statistical significance among the groups of tested datasets. A regression analysis was utilized to determine whether a linear correlation existed between the ages of patients and the number of visits they had during the 16 month of the study period and between patient ages and their rates of performed HIV testing during the study period. For statistical power reasons, only the rates of performed HIV testing among the three large main ethnicities (races), Hispanics, Blacks and Whites, were calculated and analyzed; the Asian ethnicity population was too small. We had to exclude patient visits’ data from undeclared or undocumented race groups.
Results
Demographic datasets of 5,603 patient visits of adolescent patients and young adults who sought preventive care in our facility throughout a period of 16 months were retrieved, tabulated and analyzed (Table 1).
| Study Features | Data | Analyses | Figures |
|---|---|---|---|
| Period of study | 01/01/15-04/30/16 | - | - |
| Total # of patientvisits during the study period | 5,603 patient visits | - | - |
| Patient age range (y) | 13-21 years | - | - |
| Gender distribution | F-2992 (53%) M-2611 [47% |
p=NS | - |
| Number [%] of declared ethnicities among all patient visits | Hispanics-2668 [48%] Blacks-978 [17%] White-109 [2%] Asian-31[0.5%] Other/Undeclared-1586 [28%] |
||
| Total # of Patients in the 3 largest declared ethnicities | 3,775 patient visits | - | - |
| Number [%] of ethnicities among the 3 largest declared ones | Hispanics-2668 [71%] Blacks-978 [26%] White-109 [3%] |
p<0.05 compared to other p<0.05 compared to other |
- |
| % performed HIV testing in the 3 Main patient ethnicities | Whites-29% Hispanics-20% Blacks-18% |
P<0.05-compared to other p=NS-compared with blacks |
- |
| Age of patients in relation to general number of visits per month | InverseLinear Correlation | p<0.05 R. Sq. (Adj.) – 97% |
Figure 1 |
| % performed HIV testing in Relation to Age | Direct Linear Correlation up to Age 19 Significant drop off from age 19 to 21. |
P<0.05 R. Sq. (Adj.)-93% P<0.05-for age 19 compared with21 |
Figure 2 Figure 4 |
Table 1: Datasets and comparative analysis.
Their ages ranged from 13 years to 21 years. Their gender distribution demonstrated no significant difference between the number of males and females (47% and 53%, respectively). Only 3,775 (67%) patient visit charts had a declared and documented specific ethnicities while 1,586 [33%] did not. Out of the 3,775 declared ethnicities, the 3 main ones were, 2668 [71%] Hispanics, 978 (21%) blacks, 109 (3%) whites, indicating a significant prevalence of Hispanics and Blacks in this area of South Bronx (p<0.05). The HIV testing rates in these 3 main ethnicities were 29% for whites, 20% for Hispanics and 18% for blacks [p<0.05; comparing whites to blacks and Hispanics; Figure 1]. There was a significant inverse linear correlation among patient ages and their number of visits during the study [p=0.000; R2Ad=97%; Figure 2]. From age 13 through age 19, there was a significant direct linear correlation among patient ages and rates of agreed to, and performed, HIV testing [p=0.000; R2Ad=93%; Figure 3]. Patient ages of 20 and 21 showed a decline in the rates of HIV testing from age 19 with a significant drop in these rates for age 21 compared with 19. [p<005; Figure 3].
Discussion
Several studies have demonstrated that HIV infection rates in gay and bisexual men are generally much lower than they were 10 to 12 years ago indicating major changes in the numbers of sex partners and the level of high-risk sexual behavior in most gay and bisexual men in most places [8]. In 2012 it was determined that NYC continued to have one of the largest HIV epidemics in the United States [9]. Yet, new HIV and AIDS diagnoses, incidents of HIV infections, perinatal infections, and deaths among persons with HIV had been declining, and the number of persons living with HIV growing. As of the end of 2012, 114,926 persons who had been diagnosed with HIV/AIDS and reported in NYC, were presumed to be still living whereas 1,578 deaths occurred [10].
Important disparities in HIV infection by sex, race/ethnicity, HIV transmission risk, geography within NYC, and poverty level, among other factors persisted in NYC in 2012. Persons newly diagnosed with HIV were largely male, black or Hispanic, young, men reporting sex with men, or persons living in impoverished NYC ZIP codes [10]. HIV diagnosis rates were strikingly high among black and Hispanic males and females relative to other racial/ethnic groups. HIV continued to be unevenly distributed across NYC, with most highburden areas also having a high proportion of impoverished residents. Disparities were also apparent in mortality and survival rates among persons with HIV. Persons living in highpoverty neighborhoods experienced more HIVrelated deaths, and had poorer longterm survival, compared with persons living in areas with less poverty [10].
Adolescents constitute a substantial and growing proportion of people with newly diagnosed HIV in the United States. The plan to increase HIV testing among adolescents and young adults is an essential strategy to combat this HIV/AIDS occurrence rate in the United States [11]. Our quality improvement-based study focused on the rates of agreement to undergoing routine rapid HIV testing among these young patients who sought preventive care based on current recommended schedule by the American Academy of Pediatrics [12]; their ages ranged from 13 years through 21 years and they were all living around our healthcare facility in South Bronx, NY. South Bronx has been known to have high-poverty neighborhoods, with communities of Hispanic and black predominance, both of which factors correlate with high rates of HIV positive people and AIDS [13]. Moreover, a statewide testing program of all newborn babies showed that in one South Bronx ZIP code, 1 in 25 mothers had the AIDS virus [14]. Thus, the socio-demographic makeup of the population in South Bronx and the fact that it had one of the highest AIDS infection rates in the country, underscores the validity and importance of our quality-based project. It should also be emphasized that while we aimed at determining our specific population compliance with early detection of HIV infection, our facility had the capability of offering guidance regarding early counselling and medical intervention as deemed necessary to improve quality of life and longevity in those who were found to be HIV positive.
The schedule for adolescent preventive care visits by the American Academy of Pediatrics indicates that one clinic visit, per each teenage year and up to age 21, is recommended [4]. However, our results showed that the rates of general pediatric preventive care visits between the ages of 13 and 21 dwindle. By contrast, the rates of agreement to be tested for HIV increased steadily up to age 19. It is unclear, based on our study, as to why there was a subsequent decline in HIV testing at ages 20 and 21. Nevertheless, the benefit of such findings may prompt our health providers to more proactively focus on older teenagers, such as 17 through 19, in getting them to comply first with their general preventive care visits schedule and also address more thoroughly any ‘no-shows’ in the future. Our basic premise is that a better compliance with a general preventive care visit at these ages yield better HIV testing rates as well.
Our results also demonstrated that white patients in South Bronx had a better compliance rate with HIV testing than that with Hispanics and blacks. While our study was not designed to answer the question as to why white patients were more compliant than the other ethnicities, it could be speculated that this disparity may emanate from differences in socioeconomic backgrounds and levels of education [15,16]. Ethnicity is strongly correlated with socioeconomic status (SES) in the U.S., where members of specific ethnic groups, such as African Americans, are disproportionately represented among the poor. Experience with children suffering from asthma has taught researchers that parents of black and Hispanic children tend to have worse compliance with preventive medications, even when insurance coverage is not an issue; they also have lower expectations for symptom control and functionality and show a tendency toward under-perception of symptoms [17]. Whether these attributes also affect their perception regarding HIV testing, remains to be elucidated.
In summary, this study determined that the yield of HIV testing in South Bronx tends to become higher with older teenagers and the white ethnicity. Differences in SES among ethnic groups are likely to influence disparities regarding compliance with preventive care needs. A better understanding of these SES-related cultural and behavioral pathways is essential when attempting to mitigate such disparities. However, the interactions among all factors that may affect disparities are very complex and difficult to evaluate. While vigorous efforts to address ethnicity related, and SES related, poor compliance with HIV testing are ongoing, acknowledging the potential impact that these factors exert on preventive care medicine in general and HIV testing in particular is paramount.Thus, current compliance with the requirement to have one visit for preventive care per each year of adolescent life may be difficult to achieve due to behavioral, cultural and SES issues in specific communities. Nevertheless, our role as health care providers is to engage in proper patient and family interaction in order to improve disease prevention and promote quality care and patient safety.
References
- Centers for Disease Control and Prevention (2008) HIV prevalence estimates: United States. Morb Mortal Wkly Rep 57:1073–1076.
- Branson BM, Handsfield HH, Lampe MA (2006) Revised recommendations for hiv testing of adults, adolescents, and pregnant Women in health-care settings. Morb Mortal Wkly Rep55: 1-17
- Centers for Disease Control and Prevention (2008) HIV surveillance report.
- Committee on Pediatric AIDS (2011) Adolescents and HIV infection: The pediatrician’s role in promoting routine testing.Am Acad Pediatrics 128:1023–1029.
- Weintrob AC, Giner J, Menezes P (2003) Infrequent diagnosis of primary human immunodeficiency virus infection: Missed opportunities in acute care settings. Arch Intern Med 163:2097–2100.
- Bartlett JG, Branson BM, Fenton K (2008) Opt-out testing for human immunodeficiency virus in the United States: progress and challenges. JAMA 300:945–951.
- Centers for Disease Control and Prevention (2011) HIV Surveillance - Epidemiology of HIV Infection slide set.
- Green TA, Karon JM, NwanyanwuOC (1992) Changes in AIDS incidence trends in the United States. J Acquir Immune DeficSyndr5:547-555.
- Holmberg SD (1996) The estimated prevalence and incidence of HIV in 96 large US metropolitan areas. Am J Public Health 86:642-654.
- New York City Department of Health and Mental Hygiene (2012) New York State HIV/AIDS Surveillance Annual Report.
- Grant AM, Jamieson DJ, Elam-Evans LD (2006) Reasons for testing and clinical and demographic profile of adolescents with non–perinatally acquired HIV infection. Pediatrics 117:e468-e475.
- Recommendations for Preventive Pediatric Health Care (2008) Bright Futures/American Academy of Pediatrics.
- Denning P, DiNenno E (2010) Communities in crisis: Is there a generalized HIV epidemic in impoverished urban areas of the United States?
- Bronx Community Needs Assessment Final Draft November 14, 2014.
- Crimmins EM, Hayward MD, Seeman TE (2004) Critical perspectives on racial and ethnic differences in health in late life. National Research Council (US) Panel on race, ethnicity, and health in later life; Anderson NB, Bulatao RA, Cohen B, (Eds). Washington (DC): National Academies Press (US).
- Ryan CL, Bauman K (2016) Educational Attainment in the United States: 2015; Population Characteristics Current Population Reports 20: 578.
- Forno E, Celedón JC (2009) Asthma and Ethnic Minorities: Socioeconomic Status and Beyond. CurrOpin Allergy ClinImmunol 9: 154–160.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences