Lived Experience of Multi-Drug Resistant Tuberculosis Patient; A Hermeneutic Phenomenological Study
Abay Burusie, Tafesse Lamaro, Berhe Dessalegn
1Arsi University, College of Health Sciences, Ethiopia
2Mizan Tepi University, College of Health Sciences, Ethiopia
3Adigrat University, College of Health Sciences, Ethiopia
- Corresponding Author:
- Abay Burusie
Arsi University, College of Health Sciences, Ethiopia
E-mail:babaynanaty@gmail.com; abay_burusie@yahoo.com
Received Date: May 20, 2020; Accepted Date: July 23, 2020; Published Date: July 30, 2020
Citation: Burusie A, Lamaro T, Dessalegn B (2020) Lived Experience of Multi-Drug Resistant Tuberculosis Patient; A Hermeneutic Phenomenological Study. J Prev Med Vol. 5 Iss No. 3: 09 doi:10.36648/2572-5483.5.3.09
Copyright: © 2020 Burusie A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Control of multi-drug resistant tuberculosis doesn’t rely only on the presence of effective drugs to cure it but also psychosocial and economic factors of the cases.
Methods: A hermeneutic phenomenological study design was used to explore the lived experience of patients with multidrug-resistant or extensively drugresistant tuberculosis at ALERT hospital on December 28, 2017. Purposive sampling technique was employed to recruit the study participants. A semi-structured interview guide was developed to undertake an in-depth interview. Open Code software version 4.02 was employed to make the analysis. Emergent codes were assigned to segments of the transcript that were relevant to the study objective. Finally, themes were developed from the categories. In reporting the findings, the consolidated criteria for reporting qualitative research (CORE-Q) were followed. Finally, the inter-relationship among codes, categories and themes were displayed using a diagram.
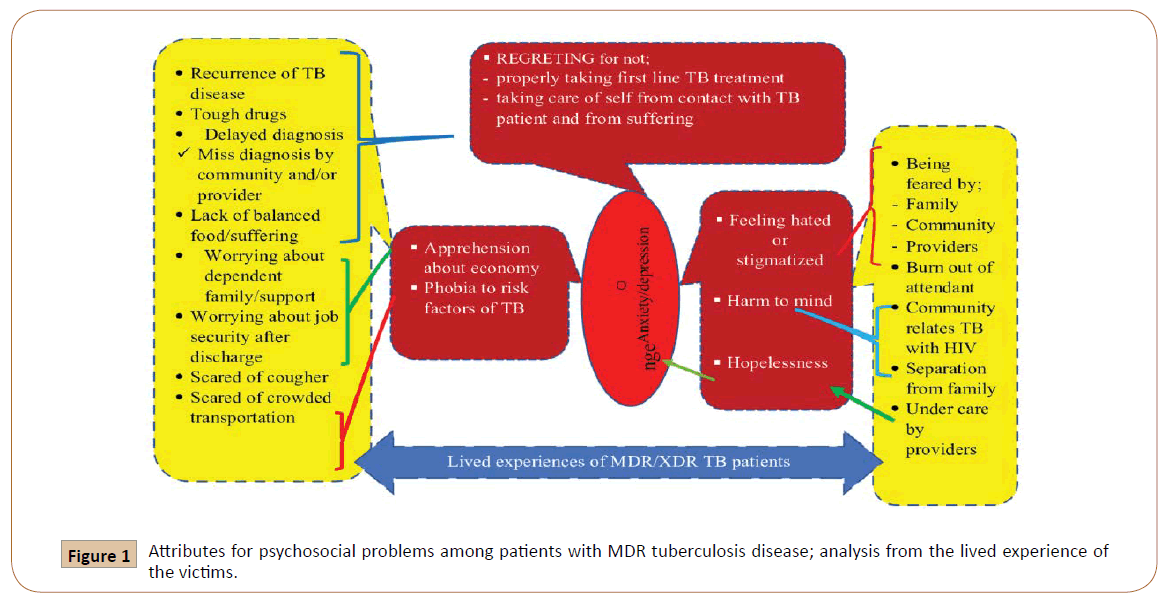
Results: Six categories were identified from the codes as contributors to psychosocial problems in MDR-TB patients. Those were; Apprehension about the economy for the survival of dependent family or self, phobia development against risk factors of tuberculosis, regretting about poor handling of life to protect self from tuberculosis, feeling hated or stigmatized, hopelessness and harm to the mind. These categories were then used to develop two major themes, namely, anxiety/depression, and intending revenge to transmit the disease to others.
Conclusion: Control of multidrug-resistant tuberculosis demands beyond the therapeutic treatment and thus, it needs to invariably include psycho-social and economic issues of the patients.
Keywords
Multi-drug resistant tuberculosis, Psycho-social, Challenges
Introduction
Tuberculosis (TB) is an infectious disease caused by the bacillus Mycobacterium tuberculosis. It typically affects the lungs (pulmonary TB) but can also affect other sites (extrapulmonary TB). The disease is spread when people who are sick with pulmonary TB expel bacteria into the air, for example by coughing [1].
Overall, a relatively small proportion (5–15%) of the estimated 2-3 billion people infected with Mycobacterium tuberculosis will develop TB disease during their lifetime. However, the probability of developing TB disease is much higher among people infected with HIV. Tuberculosis is treatable and it can be cured. But the problem, currently, is the emergence of drug-resistant tuberculosis (TB), particularly multidrug-resistant (MDR) and extensively-resistant (XDR) TB, which become a major public health problem. In 2015 alone, there were an estimated 480,000 new cases of MDR-TB and an additional 100, 000 people with rifampicin-resistant TB who were also newly eligible for MDR-TB treatment. Ethiopia is one of the 14 high burden countries with MDR TB in the world [2].
Tuberculosis is the ninth leading cause of death worldwide and the leading cause of a single infectious agent, ranking above HIV/ AIDS. In 2016, there were an estimated 1.3 million TB deaths among HIV-negative people (down from 1.7 million in 2000) and an additional 374 000 deaths among HIV-positive people. An estimated 10.4 million people fell ill with TB in 2016: 90% were adults, 65% were male, 10% were people living with HIV (74% in Africa) and 56% were in five countries: India, Indonesia, China, the Philippines, and Pakistan. Drug-resistant TB is a continuing threat. In 2016, there were 600 000 new cases with resistance to rifampicin (RR- TB), the most effective first-line drug, of which 490 000 had multidrug-resistant TB (MDR-TB).
Almost half (47%) of these cases were in India, China, and the Russian Federation. Most deaths from TB could be prevented with early diagnosis and appropriate treatment. Millions of people are diagnosed and successfully treated for TB each year, averting millions of deaths (53 million 2000–2016), but there are still large gaps in detection and treatment [3].
Multidrug resistance tuberculosis is a form of TB caused by bacteria that is resistant to treatment with at least two of the most powerful first-line anti-TB drugs, namely Isoniazid and Rifampicin. Whereas, XDR TB is a rare type of MDR TB that is resistant to Isoniazid and Rifampicin, plus any of fluoroquinolone and at least one of the three injectable second-line drugs (i.e. Amikacin, Kanamycin, and Capreomycin) [4].
The appearance of drug-resistant TB is not a recent occurrence, rather, an unfortunate and expected consequence of the adaptation of M. tuberculosis to the use of antibiotics. The progressive development of drug resistance can be expected if we fail to improve treatment and control measures for TB [5].
Successful treatment outcome is low in MDR TB patients than drug-susceptible TB patients [6].
Adverse events of the second-line treatments make the management of MDR/XDR TB very difficult. Hearing loss and nephrotoxicity are the most frequent and serious adverse reactions. Administration of injectable second-line treatment which needs many months to complete the doses is unpleasant and unwelcoming especially to children and emaciated patients [7].
Additionally, being diagnosed with MDR-TB and undergoing treatment imposes significant psychological, social and economic stress on patients [8].
Financially, MDRTB patients were worst suffered as compared to drug-susceptible TB while both groups are affected socially due to the social stigma attached to the disease [9].
By the time the diagnosis is reached, patients’ or their families’ financial and emotional resources were often depleted. Side effects of the drugs were reported to be severe and debilitating, and patients expressed the burden of care and stigma on the social and financial viability of the household. Family caregivers were crucial to maintaining the mental and physical health of patients but reported high levels of fatigue and stress marking that the barriers to patient adherence were fundamentally social, rather than medical alone [10].
Studies recommend that psychosocial support is a crucial component of treatment for MDR-TB in order to ensure the completion of complicated treatment regimens and enable psychosocial rehabilitation after treatment [11].
It was identified that home-based care better alleviates the problems of psychological, social and economic than institutionbased care as home-based care is perceived as safe, conducive to recovery, facilitating psychosocial support and allowing more free time and earning potential for patients and caretakers [12,13,14].
Studies conducted so far in Ethiopia were quantitative studies that majorly focus on determinants of treatment outcome of TB and they invariably reported low treatment success rate [15-18]. Thus, the studies were limited to quantifying the problem and recommending very vaguely. Thus, this study will dig out the lived experience of MDR TB patients so as to identify psychosocial factors that might contribute to poor quality of life [9] which in turn, understandably, contribute to poor treatment outcome and further transmission of the disease to the community at large and to family members particularly.
Methods
Study setting
The study was conducted in ALERT hospital. ALERT is a medical facility on the edge of the west of Addis Ababa. It is specializing in Hansen’s disease, also known as “leprosy”. Its name was obtained from the acronym of the All Africa Leprosy Rehabilitation and Training Center, but the official name is now expanded to include tuberculosis: All Africa Leprosy, Tuberculosis, and Rehabilitation Training Centre. Also at ALERT is the Armauer Hansen Research Institute (AHRI), founded in 1970, specializing in leprosy research [19]. The Alert MDR-TB Clinic in Addis Ababa, Ethiopia is the central referral hospital for multi-drug resistant tuberculosis until very recently before the expansion of MDR -TB centers to some selected health facilities and is currently the only center for extensively drug-resistant (XDR) tuberculosis.
Design
A hermeneutic phenomenological study design was employed to explore the lived experience of patients with MDR/XDR-TB on December 28, 2017.
Study participants
The study participants were ambulatory MDR/XDR-TB patients who were on treatment or having followed up after cure at ALERT TB clinic.
Sampling technique
Purposive sampling technique was employed to include both sexes (male and female) and to involve participants who were residents of Addis Ababa city and participants referred from out of Addis Ababa. Participants across the duration of the treatment course, ranging from early months to treatment completed period, were included to appreciate experiences across the whole treatment duration.
Sample size
Five in-depth interviews were done. Four in-depth interviews were taken on MDR TB cases and one was on XDR TB case. Sampling to saturation or theoretical saturation approach [20] was not applied in this study.
Method of data collection
First, the interview guide which was a semi-structured questionnaire and had main questions and probing questions were developed. Data were collected by face-to-face in-depth interviews. Interviews began with the collection of basic information including sex, age, occupation, marital status, the residence of the patient and duration since treatment started. The main questions encompass transition questions like, can you tell me about your illness? and probed by, what type of TB is that? And what does MDR/XDR TB mean? The core questions comprehend; how do you see being MDR TB patient? Followed by probing questions like, what are the major challenges MDR/ XDR TB patients face? And what do you think has caused you to contract TB disease? With probing question of, what is your contact history with TB patients either in family or neighbor? The interviewer was the corresponding author. Field notes which remind core descriptions and emotional expressions of the participants were taken while an audio record was also secured.
Data analysis
The interview that was done by the Amharic language was first transcribed verbatim on hardcopy and then translated into the English language in softcopy. The translated word files were separately saved for each interview. Then, the word files were saved as plain text and imported to Open Code 4.02 software for coding. Subsequently, selective coding was done, i.e. emergent codes were assigned to segments of the transcript that were relevant to the study objectives. After completing coding, categories were ascribed to the developed codes. Finally, themes were developed from the categories. In writing the results, quotes and paraphrases were supplemented by observations that were jotted down as field notes. In reporting the findings of this study, the authors followed the consolidated criteria for reporting qualitative research (CORE-Q) which is a 32-items checklist [21].
Result
In this qualitative study, 3 females (2 with MDR and 1 with XDR TB) and 2 males (both with MDR TB) were involved. The age range of the participants was 14 to 38 years. By residence, 2 were from Addis Ababa and the remaining were referred cases from outside of Addis Ababa. Participants’ duration on treatment at the time of the interview ranged from as early as 1 month to treatment completed duration, i.e. 20 months. The Basic information of study participants is shown in Table 1.
| S.No | Sex | Age (in completed years) | Occupation | Marital status | Residence | Treatment duration (in completed months) |
|---|---|---|---|---|---|---|
| 1 | Female | 14 | Student (grade 7 drop out) | Single | Harer/Babile | 3 |
| 2 | Female | 33 | Housewife | Married | Addis Ababa/Jan Meda | 20 |
| 3 | Male | 26 | Daily laborer | Single | Addis Ababa/Mesalemia | 2 |
| 4 | Male | 38 | Daily laborer | Widower | Burayu/Ashewa Meda | 2 |
| 5 | Female | 18 | Student | Single | Metu | 1 |
Table 1. Basic information of patients with MDR tuberculosis involved in an in-depth interview, ALERT hospital, Addis Ababa
From this study, two themes that majorly remark psychosocial problems were identified. These were; anxiety/depression and the potential of intending revenge. In the subsequent sections, categories identified for each theme will be elaborated employing quotes from the statement of participants and researchers’ observations.
Anxiety
Anxiety was one of the themes that emerged from this study. The study participants’ anxiety was manifested, for instance, by apprehension about both current and future economy for the survival of dependent family members and self. One participant said, “My mom is very aged and weak. Previously, it was me who used to support her by working as a daily laborer. Staying here, I worry about my mother who is facing ups and downs to send my children school. While staying here, I am much stressed about my family on how to support them being discharged sooner”. (Male, MDR-TB patient, Age 38 years)
It was also found that apprehension about one’s economy to survive may contribute to the delayed response of MDR TB patient to referral to MDR TB treatment center to ensure timely initiation of the treatment. The following is a quote from one of the study participants; “I came to the MDR TB center late after one month of receiving my referral paper. Because I was told at the health center that I was going to be admitted for two months, and I was worried that who would support me if I am admitted for that long”. (Male, MDR-TB patient, Age 26 years)
Worrying about how to economically survive after discharge from the center where they are served with shelter and meal for free was also identified as a problem among MDR-TB patients. A participant said, “I don’t have relatives that can support me if am discharged now. The doctors let me stay here in the center despite the fact I should leave and look for a rental house by this time”. (Male, MDR-TB patient, Age 38 years)
Another participant with the same worry stated his apprehension about the future economy as, “Paying house rent! You think about what to pay for house rent after being discharged, you also think about how you can get food to eat. Here food is served for free; we don’t pay for the bed also. But when you think about what will happen after discharge, you get much worried”. (Male, MDR-TB patient, Age 26 years)
Additionally, the development of phobia to risk factors of tuberculosis and regretting failing taking self-care were found potential markers of anxiety among MDR-TB patients.
Phobias identified as those developed to risk factors of TB by the MDR-TB patient include being scared of coughers and crowdedness. A participant described fearfulness to coughers as, “let alone when I see my children coughing, I even get very scared when I see other people around me coughing”. (Female, MDR-TB patient, Age 33 years)
Participants expressed also that they fear crowded transportation like city bus and “Higher” taxi because one share breathes of others which is the means of TB transmission. A woman bitterly expressed about crowded transportation as “I was caught by this disease surely from in transportation. Because this disease was not present in my area; this kind of thing was not present in my family. For me, it is the transport! [Heavily shaking her head]. I definitely believe that this disease caught me in transportation. There is a high chance for the community to breath-in the highly contaminated air in transportation”. (Female, MDR-TB patient, Age 33 years)
Regret was also identified as a category that may fit the anxiety theme. The foundations of regret that were identified from the study participants include; regretting for not properly taking the first-line TB treatment during previous TB illness, and regretting for not taking care of self from contact with TB patient, and from lack of balanced food and exposure to heavy-duty such as being daily laborer of construction activities which causes body to suffer.
Recurrence of TB disease, suffering from side effects of MDR/XDRTB drugs, and delayed diagnosis of the disease either because of miss diagnosis by providers and/or community instigated the participants to regret not properly taking the first-line drugs. A child participant regretted her failure to take TB prophylaxis prescribed for her by saying, “The medication is very ugly! I don’t know, but it was very tough. Previously I had completed 6-month’s treatment for TB and it returned again after 8 years. Then swellings appeared here and here [touching under her neck] and under my armpit. Then the sample was taken from the swelling. In the meantime, my leg has become swollen. We left aside swelling on my neck and seek treatment for my swollen leg. X-ray of my leg was taken. Then it was said blood coagulation and I was admitted to hospital for 20 days. Then we [I and my mom] said OK, the swelling on my neck could also be a sign of blood coagulation. Then after I finished my injections for my leg I was sent home with tablets to sallow for three months. After I went home again I didn’t get improved and was unable to be as before. When I saw a meal with my eyes, I used to vomit. I nauseate; I didn’t eat food; I didn’t take soup; in the morning I was vomiting bile. Then I became very weak. Then, my mom took me to the hospital again and I was re-admitted. Then one physician ordered sputum examination and it was identified as drug accustomed TB. Otherwise, it was not identified easily. Actually, I was careless. I thought it is an easy disease. When I think now, it was my mistake. I stopped taking the drugs, white color tablets, after taking it only for a few days which were given to me for TB prophylaxis”. (Female, MDR-TB patient, Age 14 years)
A participant with MDR-TB responded to a question, had you properly taken and completed your first-line TB drugs, as “No! I don’t want to lie to anyone at this point. Because of my weakness, sometimes I used to interrupt as I went away from home to other places for business purposes”. He was regretting that the disease wouldn’t have come again being worsened (becoming MDR-TB) had he had taken his first-line TB drugs properly during previous illness by saying, “The reason why I didn’t properly take the drug during first disease staying at my home was because of my hardship life. Because I am young, I run there and here working as a daily laborer, and prioritizing my work to my health lastly brought me this disease. Had I had taken my drugs properly and completed my drug it (MDR-TB) wouldn’t have come”. (Male, MDR-TB patient, Age 26 years)
Study participants also expressed their regrets for failing to refrain from contacting TB patients. One participant, who took various medications for a long time for her MDR TB and later diagnosed as XDR-TB, expressed her regret as, “In my neighborhood, there was one girl who was sick of TB. I frequently go to her home, chat with her, eat food and drink with her. When she coughs and sneezes she didn’t take care. But I didn’t know that she was sick of TB. Later, it was found that she had taken two rounds of six months of' TB treatment. She used to take the drugs irregularly. For the third time when she was examined after I told the doctors about her, she was found she had MDR TB and now she is taking the drugs”. (Female, XDR-TB patient, Age 18 years)
Another participant regrets contact with TB patient and failure to protect herself as, “Before me, my brother was sick and I was taking care after him. Two years later, the disease has come to me too. Now he has passed away. Had I known his illness was TB, I would have taken care of myself by wearing a mask. I didn’t know he had TB because his TB was identified at the end when he was imminent die”. (Male, MDR-TB patient, Age 26 years)
Regretting about suffering from a lack of a balanced diet was stated as “For me, it is physical suffering that caused me TB. If there will be suffering no doubt that it will come again too. You have to care for yourself with balanced food. You have to eat your food timely. You need to get an egg etc”. (Female, MDR-TB patient, Age 14 years)
Emphasizing the importance of a balanced diet, another participant said, “Care is food. In the morning you need to get a good meal. It [MDR-TB treatment center] provides only tea and bread. It rarely brings “Firfir” [local food prepared by mixing “Injera” with sauce] once per week. Consuming tea and bread alone during breakfast time is not enough to be strong enough to take all these many drugs. We females cook additional and care ourselves. But males don’t do this”. (Female, XDR-TB patient, Age 18 years)
Another participant who had taken first-line TB treatments two times previously, he orally reported, regretted that suffering from heavy-duty brought him MDR TB and described it as, “I had completed my drugs during previous TB illnesses but as soon as I finished I went for work. So, I greedily went for work before getting rehabilitated. Unless I take drugs late in hours I didn’t interrupt at those times. It is suffering surely. When you work, these dusts inter into you. I guess it was the suffering that caused me for this disease”. (Male, MDR-TB patient, Age 38 years)
In addition to the aforementioned categories such as apprehension about the economy, phobia to risk factors and regret, feeling hated or stigmatized and harm to mind were also located to the theme of anxiety or depression.
Among the study participants, feeling hated or stigmatized were described by reporting being feared by family members, community and/or provider, and by reporting burn out of their attendants. The child participants described her life’s experience of being hated or stigmatized as, “community stigmatizes very much! [Shaking her head] because they fear the disease. Even my mother who was attending me for the first two months after I started the treatment, fears me so much. She says, go back! Don’t come close to me! [Speaking louder]. By passers cover their nose with their arm and sometimes we see them running away when they see us outside of our room. By now, because I adapted, I don’t care if they look at me with fear and run away. Rather we scoff at them saying, run! run! To escape from being eaten”. (Female, MDR-TB patient, Age 14 years)
Another participant also described her life’s experience similarly, but including her perception about providers and said it as, “Mainly being stigmatized by your family and community brings mind stress onto you. Secondly, when I bring my babies to the hospital for a checkup, every health provider around there was scared of me and my babies, and they discharged my babies by rush though I wear a mask that prevents transmission. That time I cried a lot”. (Female, MDR-TB patient, Age 33 years) The severity of stigma among MDR-TB patients in the words of another participant was quoted as, “Multidrug-resistant tuberculosis is scared more than HIV is. I don’t know the reason; the doctors even fear it very much”. (Female, XDR-TB patient, Age 18 years)
Contrarily, another participant denied any stigma from anybody saying, “There is no stigma to MDR TB patients. For example, someone who is sick can get cured. If he/she properly takes his/ her drugs and has eaten food well, he/she will be cured”. (Male, MDR-TB patient, Age 26 years)
An MDR-TB patient who was miss diagnosed as coagulopathy described the burn out of her attending family as “I used to have a checkup for my swollen leg weekly and my mom is burnt out of taking me weekly for follow up”. (Female, MDR-TB patient, Age 14 years)
Harm to mind, which may contribute to anxiety or depression was also identified. One study participant described how being MRD-TB patient harmed her mind saying it out as “People give you different opinions. They say, it comes from HIV or it may change to HIV blab and this highly harms your mind”. (Female, MDR-TB patient, Age 33 years)
Revenge
The second theme that was identified from this study was that the potential to intend to revenge others in mass by transmitting MDR-TB disease. The ground for revenge maybe because of hopelessness by the MDR-TB patient secondary to perceiving being under-cared by health care providers. A participant described intending revenge as, “Now, the problem is, if you leave from here before the severity of our illness unalleviated very well, it will be a disaster. If you get annoyed with something over here and leave from here (i.e. MDR-TB treatment center) of a sudden, you may harm many individuals who are very useful to the nation. For instance, officials who are rushing for office in the morning sometimes use the train to save time instead of waiting for a taxi. This means, if you get into the train, on the train you can easily contaminate all on the train”. (Male, MDR-TB patient, Age 26 years)
The inter-relationship among codes, categories, and themes analyzed is diagrammatically displayed in Figure 1.
Discussion
This study has tried to understand the lived experience of MDR/ XDR-TB patients during their treatment course with regard to psychosocial factors through in-depth face-to-face interviews. However, it is deficient in that it didn’t include the view of health care providers about the patients as the behavior of health care providers, imposed by the fears of infection, contributed to discrimination of patients in the facility [22] and which, of course, was also disclosed by the study participants of this study. In spite of its many limitations, however, the experience of MDRTB patients that the study has revealed cannot be undermined. To our knowledge, a study of the life experience of the MDR-TB patient which is imperative to the prevention and control of the disease was lacking. Even though it is not reasonable, in spite of all the limitations of the study, to limit the number of themes that might emerge from such study, the two major themes developed, anxiety/depression and intending revenge will be discussed hereafter. Because an extremely confusing area is the intricate relationship between the anxieties and the depressions [23], in this study, both were reported as one emerging theme of the psychological problem among the MDR-TB patients without segregating their contributors.
Here, apprehension about the economy was identified as a contributor to anxiety/depression. Previous studies indicated that financial hardship has been identified as a major contributor to loss to follow up of MDR-TB patients [24]. Understandably, having a source of income is desperately required for survival. On the other hand, the inability to work and generate income, like the one that is seen among MDR-TB patients who are admitted to MDR-TB treatment center/clinic, imposes stress on one’s life. Financially, MDR-TB patients are worst suffered because of the treatment takes longer time and side effects of the drug is unbearable to most of the cases to generate income, and delayed diagnosis because of miss diagnosis either by health care providers or family had already caused depletion of their resources at the time of correct diagnosis [7-9]. If this worry of the economy is excessive and out of control, it can end up with Generalized Anxiety Disorder (GAD) [25] and obviously, the problem will be compounded if there are dependent family members in addition to one’s own difficult situation. In this study, males were identified clearly expressing their worry about the economy of the dependent family. In Ethiopia, TB treatment success rates at various areas were reported very low [15-17] and it would be much very low if treatment success rate was computed for MDR-TB cases which need a longer duration of treatment and in which patients are forced to face multiple side effects of second-line treatment [6]. Comparing gender, studies of TB treatment outcome in Ethiopia identified that males have a lower treatment success rate as compared to female counterparts [15,17]. This may imply that the reason for the lower treatment success rate among male patients may be because males shoulder the economy of the family. Being anxious when failing to meet for self and dependent family members can expense males to become treatment unsuccessful. Additionally, they may leave the MDR-TB treatment center prematurely to combat the economic challenge before culture conversion from positive to negative and hence, disseminate the disease to the community. This may need to design income generation means for ambulatory MRD-TB patients while they are staying in the treatment center.
As it was indicated, MDR-TB patients may also suffer from phobia to coughers and crowded means of transportation because they believe that all the aftermaths of the disease they experienced or are experiencing were caused by exposure to these factors. This phobia may lead to post-traumatic stress disorder (PTSD), which is a condition that causes flashbacks or anxiety as the result of a traumatic experience [23]. Of course, the patients’ fear of chronic coughers is reasonable as close contact with such an individual is a risk factor for the transmission [26]. Similarly, being scared of crowded public transportation is justifiable as studies indicate that such conditions facilitate TB transmission [27,28]. This indicates that MDR-TB patients highly require psychological support to endure phobias developed against the risk factors which they associate with the hardship they experienced with the drug side effects, pain from the disease and social stigma [8] by educating on prevention methods.
The regret that originates from a failure to protect self from TB disease because of not knowing the characteristics of the disease and its mode of transmission was also reflected by the study participants. Psychosocial support is a crucial component of treatment for MDR-TB in order to ensure the completion of complicated treatment regimens and enable psychosocial rehabilitation after treatment to protect MDR-TB patients from depression [11].
The opportunity of becoming hopeless among MDR-TB patients needs to be foreseen and given due attention. As it is clearly noted, drugs for the treatment of MDR-TB are extremely unpleasant and side effects are unbearable [7]. That is why the 14-year girl expressed drugs for treatment MDR-TB as, “the drugs are very ugly!” Unless responses to these pains and suffering can be managed they may provoke MDR-TB patients to revenge others by transmitting the disease [29].
It was described that, from one of the study participants in this study, intending revenge to transmit the disease by typically choosing crowd in case of perceiving under care by provides is likely. Undeniably, there are times that health care providers could under care for their patients. An MDR-TB patient who is annoyed by the under care from the provider may committee revenge intentionally. Because the constraints imposed by providers or societies may instigate hopeless in MDR-TB patients to commit revenge by intentionally exposing others [30].
Health care providers’ act towards MDR-TB patients was blamed by the participants as the providers don’t want an MDR TB patient to stay longer time around them even the patients wearing their nasal mask. This suggests that providers’ fear of infection could contribute to stigma and hindrance to the accessibility of care and support services [22]. This also implies that unless a strong protective method, other than a nasal mask that providers themselves trust its effectiveness devised, the fear of providers that elicits a feeling of being stigmatized by MDR-TB patients will incessantly be the challenge to TB control.
Conclusion
Control of MDR-TB spread demands beyond the therapeutic treatment of the patients. Therefore, psychological therapy and designing income generation mechanisms for MDR-TB patients while they are at the treatment center are commendable.
Ethical consideration
To ensure the ethical sanity of the study, permission letter was obtained from the school of public health, Addis Ababa University and presented to the office of medical director at ALERT hospital. Thereafter, the permission letter was directed to the head of ALERT TB clinic. Study participants have introduced the purpose of the study and assured that the interview incurs no harm as it remains confidential and will not be used for another purpose than the study’s objectives. To maintain privacy, the interview was undertaken in an open-air where other person closing to the interview area can easily be seen and prohibited to come closer. Identification (name) of the participants was omitted both during the interview audio record and while the basic information was being filled out. The participants were also informed that the audio recorder would be used because each and every word they raise is useful and shouldn’t be missed. Ultimately, informed consent was obtained verbally before commencing the interview. For one child participant, assent was obtained describing the purpose of the study as was made to the other adults who participated in the interview.
Consent to publish
At the end of each interview, participants were individually asked whether they are willing if the study is published and none of them objected to publishing the work as far as their name is not included or specified.
Availability of content and materials
All the audios, transcriptions and translations are kept and can be made available based on a request by the publisher.
Conflict of interest
The authors declare that they have no any conflict of interest
Acknowledgement
The authors would like to thank the study participants for their willingness to take part in the study
Quick look
Current knowledge
Studies have invariably reported that the treatment success rate of multi-drug resistant tuberculosis is very low as compared with the treatment success rate in patients of drug-susceptible tuberculosis and the global target. Demographic and clinical determinants of unsuccessful multi-drug resistant tuberculosis treatment outcomes are also identified.
What this paper contributes to our knowledge
Multi-drug resistant tuberculosis patients who were on treatment course experienced multiple psychosocial and economic challenges. Psychosocial and economic challenges of multi-drug resistant tuberculosis patients had implications for tuberculosis control.
References
- CDC (2013) Core Curriculum on Tuberculosis: What the Clinician Should Know[Online]. Centers for Disease Control and Prevention (CDC); National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of Tuberculosis Elimination.
- WHO (2016a) Global tuberculosis report Geneva, World Health Organization.
- WHO (2017) Global tuberculosis report, Geneva, World Health Organization.
- WHO (2013) Definitions and reporting framework for tuberculosis+IBM-2013 revision, Geneva, World Health Organization.
- FAUCI AS (2008) Multidrug-resistant and extensively drug-resistant tuberculosis: the National Institute of Allergy and Infectious Diseases Research agenda and recommendations for priority research. J Infect Dis 197(11): 1493-1498.
- Orenstein EW, Basu S, Shah NS, Andrews JR, Friedland GH, et al. (2009) Treatment outcomes among patients with multidrug-resistant tuberculosis: systematic review and meta-analysis. Lancet Infect Dis 9: 153-161.
- WHO (2016) WHO treatment guidelines for drug-resistant tuberculosis 2016 update, Geneva, World Health Organization.
- Morris MD, Quezada L, Bhat P, Moser K, Smith J, et al. (2013) Social, economic, and psychological impacts of MDR-TB treatment in Tijuana, Mexico: a patient's perspective. Int J Tuberc Lung Dis 17: 954-960.
- Sharma R, Yadav R, Sharma M, Saini V, Koushal V (2014) Quality of life of multi drug resistant tuberculosis patients: a study of north India. Acta Med Iran 52(6): 448-453.
- Isaakidis P, Rangan S, Pradhan A, Ladomirska J, Reid T, et al. (2013) ‘I cry every day’: experiences of patients co‐infected with HIV and multidrug‐resistant tuberculosis. Trop Med Int Health 18(9): 1128-1133.
- Acha J, Sweetland A, Guerra D, Chalco K, Castillo H, et al. (2007) Psychosocial support groups for patients with multidrug-resistant tuberculosis: five years of experience. Glob Public Health 2(4): 404-417.
- Brust JC, Shah NS, Scott M, Chaiyachati K, Lygizos M, et al. (2012) Integrated, home-based treatment for MDR-TB and HIV in rural South Africa: an alternate model of care [Perspectives]. Int J Tuberc Lung Dis 16(8): 998-1004.
- Shin S, Furin J, Bayona J, Mate K, Kim JY, et al. (2004) Community-based treatment of multidrug-resistant tuberculosis in Lima, Peru: 7 years of experience. Soc Sci Med 59(7): 1529-1539.
- Luyirika E, Nsobya H, Batamwita R, Busingye P, Musoke W, et al. (2012) A home-based approach to managing multi-drug resistant tuberculosis in Uganda: a case report. AIDS Research and Therapy9(1): 12.
- Tessema B, Muche A, Bekele A, Reissig D, Emmrich F, et al. (2009) Treatment outcome of tuberculosis patients at Gondar University Teaching Hospital, Northwest Ethiopia. A five-year retrospective study BMC Public Health 9: 371.
- Asebe G, Dissasa H, Teklu T, Gebreegizeabhe G, Tafese K, et al. (2015) Treatment outcome of tuberculosis patients at Gambella Hospital, Southwest Ethiopia: three-year retrospective study. J Infect Dis Ther 3: 211.
- Jemal M, Tarekegne D, Atanaw T, Ebabu A, Endris M, et al. (2015) Treatment outcomes of tuberculosis patients in Metema hospital, Northwest Ethiopia: a four years retrospective study. Mycobact Dis 5: 4.
- Tefera F, Dejene T, Tewelde T (2016) Treatment outcomes of tuberculosis patients at Debre Berhan Hospital, Amhara Region, Northern Ethiopia. Ethiop J Health Sci 26: 65-72.
- Wikipedia, The Free Encyclopedia. ALERT (medical facility).
- Green J, Thorogood N (2018) Qualitative methods for health research, sage.
- Booth A, Hannes K, Harden A, Noyes J, Harris J, et al. (2014) COREQ (consolidated criteria for reporting qualitative studies). Guidelines for reporting health research: a user's manual 214-26.
- Bieh KL, Weigel R, Smith H (2017) Hospitalized care for MDR-TB in Port Harcourt, Nigeria: a qualitative study. BMC Infect Dis 17: 50.
- Griez EJ, Faravelli C, Nutt D, Zohar J (2001) Anxiety disorders: an introduction to clinical management and research, Wiley.
- Shringarpure KS, Isaakidis P, Sagili KD, Baxi RK, Das M, et al. (2016) “When treatment is more challenging than the disease”: a qualitative study of MDR-TB patient retention. PLoS One 11(3): e0150849.
- National Institute of Health (2016) Generalized Anxiety Disorder: When Worry Gets Out of Control. National Institute of Mental Health.
- Mulu W, Mekkonnen D, Yimer M, Admassu A, Abera B (2015) Risk factors for multidrug resistant tuberculosis patients in Amhara National Regional State. Afr Health Sci 15: 368-377.
- Campos OH, Lama AB, Sandoval NR, Mateo MM (2010) Risk of tuberculosis in public transport sector workers, Lima, Peru. Int J Tuberc Lung Dis 14: 714-719.
- Zamudio C, Krapp F, Choi HW, Shah L, Ciampi A, et al. (2015) Public transportation and tuberculosis transmission in a high incidence setting. PLoS One 10(2):e0115230.
- Barash DP, Lipton JE (2011) Payback: Why we retaliate, redirect aggression, and take revenge, Oxford University Press. Front Psychol 7: 2062.
- Giardini F, Conte R (2015) Revenge and conflict: Social and cognitive aspects. Conflict and Multimodal Communication, Springer pp: 71-89.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences