Prospective Randomised Study Comparing Outcome Case of Hemorrhoids after Ligasure and Stapler
Hassan Awad Saad*, Kamal Rabie, Mohamed Eraky, Hassan Ashour, Mostafa M Elaidy and Ahmed M Yehia
Department of Surgery, Zagagig University, Zagagig, Egypt
Corresponding Author:
- Hassan Awad Saad
- Department of Surgery, Zagagig University, Zagagig, Egypt,
- E-mail:ebramos_2010@yahoo.com
Received date: January 05, 2023, Manuscript No. IPJPM-23-15594; Editor assigned date: January 09, 2023, PreQC No. IPJPM-23-15594 (PQ); Reviewed date: January 18, 2023, QC No IPJPM-23-15594; Revised date: January 25, 2023, Manuscript No. IPJPM-23-15594 (R); Published date: February 03, 2023, DOI: 10.36648/2572-5483.8.1.185
Citation: Saad HA, Rabie K, Eraky M, Ashour H, Elaidy MM, et al. (2023) Prospective Randomised Study Comparing Outcome Case of Hemorrhoids after Ligasure and Stapler. J Prev Med Vol.8 No.1:185
Abstract
Aim: It has been shown that for the diathermy and scissor have harmful effect and complicated of pain that little with Harmonica and Ligasure in anal surgery especially hemorrhoidectomy, so in this study we compare the Ligasure with this stapling debate.
Methods: 50 patients had 3rd to 4th degree piles were grouped to undergo LigaSure™ or stapling hemorrhoidopexy for piles hemorrhoidectomy. In Zagazig University, Surgical department parameters investigated pain, satisfaction or residual and recurrence. Post-operative course and analgesia.
Results: Equal results in all most analyzed of both groups. Patient satisfaction (P- value=1), Postoperative pain scores (P-value=0.99), and self-activity satisfaction (P- value=0.99). All equal in two groups. No major difference except in investigation.
Conclusion: Two methods can be used safety in two groups.
Keywords
Technical handling; Hemorrhoidectomy; Patient work recovery
Introduction
Using the diathermy and dissector may be the cause of pain and harmful effect on the tissue. The operation can be very painful [1] and take long time for healing and suffering more than 6 weeks [2]. This force the surgeon to create or develop new techniques and modifications to decrease the pain and rapid recovery. Operations with stapler has advantage of less operative pain and rapid recovery than the diathermy and scissor cutting hemorrhoidectomy done with diathermy or scissors cutting methods [3–10] but it is difficult to be used in fourth degree piles, and/or more skin appendages so, diathermy suitable for cutting without pain limitation [11] also the one of its disadvantage is the recurrence. As the head more fitting into the tissue stapler founding, instead the diathermy or Ligasure are not limited by amount of tissue so, both were used in patients with for 4th degree piles or excess skin tag. Little pain resulting both stapler and Ligasure than ordinary methods, the aim of this work is to determine ideal methods with little pain, easy technical application with advanced cases of piles.
Patients and Methods
We had 50 patients suffering from symptomatic 3rd and 4th degree piles in Zagazig University Surgical Department. According to ethics in our study all patients were signed on ethics approval. Patients were divided into group 1 randomised to be operated by stapler for piles excision (hemorrhoidectomy) (group 1, n=25) or group 2 by LigaSure™ technique for piles excision (hemorrhoidectomy) (group 2, n=25). All subjected to the power test; Standard Deviation (SD) done in 20 patients of each group in mean pain score, with 80% power at 5% of the level was noticed differences. For patient characteristics, refer to Tables 1 and 2. 5 cases 4 of group (1) 1 of group (2) we can’t follow-up examination (removed from the schedule). All five farther patients’ accommodation far from the hospital more than 30 km. Others 5 recruited.
Table 1: Patient characteristics.
| Ligasure | Stapler | |
|---|---|---|
| No | 25 | 25 |
| Mean age | 48 (28-82) | 11 |
| Female | 12 | 58 (40–71) |
Table 2: Hemorrhoids staging and associated finding.
|
|
Ligasure |
Stapler |
|---|---|---|
|
Piles |
9 |
10 |
|
2nd to 3rd degree |
13 |
14 |
|
3rd degree only |
1 |
1 |
|
3rd to 4th degree |
2 |
1 |
|
4th degree only |
|
|
|
Progress prolapse |
|
|
|
Partial prolapse |
15 |
10 |
|
Complete prolapse |
5 |
8 |
|
Skin appendage |
7 |
10 |
|
Fissure |
3 |
0 |
|
Itchin |
1 |
1 |
Preoperative assessment
- Full history.
- Examination including proctosigmoidoscopy.
- Routine laboratory examination. According to finding proctosigmoidoscopy the procedure were done on a patients study form.
- Unsuspected malignant mass or malignant ulcer, no differences in the distribution the hemorrhoid staging.
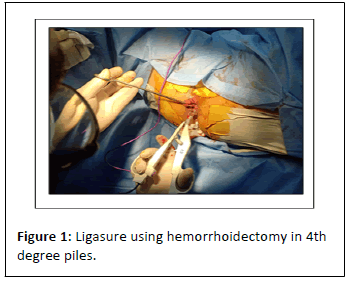
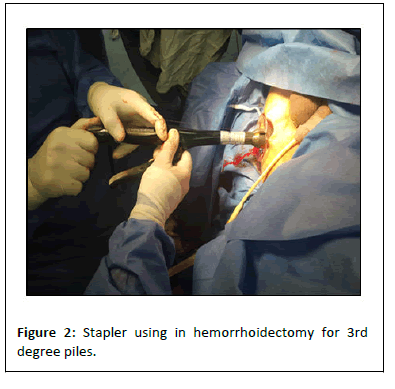
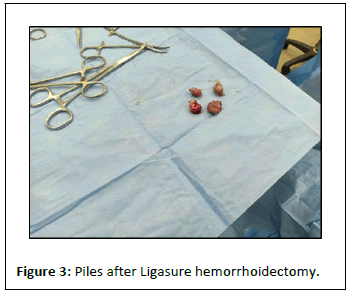
We used the stapling as described before with the Proximate® PPH stapler for residual prolapsing tissue or skin appendages. In 9 patients (36%) the diathermy was used with stapler (Table 3). By Milligan–Morgan technique Ligasure™ hemorrhoidecto -my was used. A small incision 2 cm was made at mucocutan -eous junction; along the dermato-cutaneous junction planes dissection by Ligasure™ using the smaller instrument about (18 cm). Six patients (24%) operated by this way and we proceed to segmental plastic reconstruction if associated prolapse piles (Fansler-Arnold). This procedure depending on skin and subcutaneous full thickness flab moving to cover the defect if associated anal stricture (rhomboid, trapezoid, cone shap…)
Table 3: Surgical procedures.
| Ligasure | |
|---|---|
| Classic Milligan–Morgan | 19 |
| Additional procedure | |
| Plastic flab | 6 |
| Stapler | |
| Stapler | 16 |
| Another procedure | |
| Segmental Milligan–Morgan, or skin tags | 9 |
Operation time and intraoperative steps were detected on a questionnaire. Complicated routine postoperative analgesia e.g. Diclofenac acid (3 mg× 50 mg) or ibuprofen (tid 400 mg) or Opiates in severe pain. Metronidazole 500 mg tid tab was given. Patients routinely laxative. During the hospital time and after discharge, duration of pain and analgesic therapy were recorded during hospital time. From postoperative first day 1 to 3 weeks daily recording the pain, their intake of analgesia, the recovery to personal activity percent, recorded (0-100 percent), for pain relieved with such treatment were by visual analog scales that from 0 to 10. A follow-up was up to six weeks all history, pain (visual analog scale, 0–10) and level of personal activity (0–100 percent) all detected on a separate sheet patients with self-good recovery. At the end results the duration of operating time was subjected to T-test, Pearson’s chi-squared test. Statistical software R1.9.1 (ISBN 3-900051-05-4) are expressed by mean,median and range near in all groups. Wilcoxon two-sample test used for statistical significance done for every day. Then the P values were recorded.
Results
No significant differences was detected after operation (P=0.19). Significant in the duration of operation than the other cases found in the six cases with combined anodermal flap plasty and Ligasure™ hemorrhoidectomy as were technical handling had little complicated in 12%, 24%, respectively (P=0.55, (Table 4). In post-operative results (Table 5) were controlled by the relieve satisfaction in 96% of the cases in the Ligasure™ 88% of but in the stapler group (P=0.44). Take attention without favorable level of significant advantage.
Table 4: Operative time.
|
|
Ligasure |
stapler |
|---|---|---|
|
All |
23/26 (10–80) |
20/21 (6–54) |
|
Procedure |
18/20 (10–37) |
15/18 (6–40) |
|
Combined procedure |
40/44 (20–80) |
25/25 (15–54) |
|
Note: Values are median/mean (range). P-value=0.1858. |
||
Table 5: Immediate postoperative assessment of ease of handling by the surgeon.
|
|
Ligasure™ | Stapler |
|---|---|---|
| Simple | 22 (88%) | 19 (76%) |
| Slightly-awkward | 2 (8%) | 4 (16%) |
| Associated complication | 1 (4%) | 2 (8%) |
| Note: P value=0.5535. | ||
In Table 6 record the course after the all techniques. In terms of manner and timing of the first defecation no significant differences no significant differences early operation 1, complications, and hospital duration time and analgesia need (Table 7). Median pain level was scoring (Figure 1) their near relationship between two groups. P-value for two groups after complete analyses equal to 0.99. There was a tendency of the Ligasure™ patient’s preference. Mean patient satisfaction during the first 7 days (P=1, (Figure 2)) and mean gain of personal recover of the recovery, activity and satisfaction (P=0.99, (Figure 3)) were nearly the same in two groups.
Table 6: Postoperative course.
|
|
Ligasure | stapler |
|---|---|---|
| Early complication |
|
|
| Urine retened | 2 (8%) | 4 (16%) |
| Ozzing blood | 1 (4%) | |
| All | 3 (12%) | 4 (16%) |
| Days: (Mean range) | 2/3 (1–5) | |
| First defecation |
|
|
| Suppository/enema | 6 (24%) | 8 (42%) |
| Spontaneous | 19 (76%) | 17 (68%) |
| Hospital time | ||
| Days: Median | 5/5 (2–10) | 4/4 (2–10) |
Table 7: Analgesic requirement
| Opiate | 6 (24%) | 8 (32%) |
| Morphia | 1 (4%) | |
| After discharge analgesia | ||
| No | 3 (12%) | 2 (8%) |
| Panadol | 1 (4%) | 1 (4%) |
| Diclofenic A | 6 (24%) | 5 (20%) |
| Tramadolic acid | 2 (8%) | 0 |
| Mean time range | 14 days | 16 days |
|
Note: Metroametazole, ibrufen and tramadol taken for all patients during hospital stay. |
||
Overall, the level of self-recovery with treatment was had no relation to the type of operative technique. The level of recover activity was clear decreased during the first few days up to 14 days, but the mean values increased gradually from 40% to 60%. Mean of activity satisfaction levels of 80% and above attained by the third week in the two groups but at the six week. Also no differences founded after follow the cases. In both groups, 84% of patients had no complaints but any findings in examination. In 92% self-recovery of with treatment still higher, and the level of recover activity was completes gained in the most patients.
Discussion
Painful dissection postoperative by diathermy or scissor makes both Ligasure™ and stapler. God methods and [12–16] alternatives prove in unselected patients with hemorrhoids disease. Postoperative Good handling, less pain and good patient’s patient satisfaction. Infact, we found nearly to the postoperative pain level, patient self-activity were the same in two groups. But, the investigations found factors had no any significant differences. Ligasure™ is preferred in handling than the stapler with respect to surgical equal of immediate postoperative result. The stapler apparent favorable in advanced cases (advanced fourth-degree piles). But Ligasure™ is had favorable immediate relieve as technical advantages stapler used if more excision or skin or mucous tissue reconstruction, instead of painful diathermy (4th degree piles).
So, Stapling not eliminate the pathology but receive it. So, the main studies about stapler deal with this point. Some studies suspect there is patients selection not “suitable” for stapling attention toward hemorrhoids cases, but usually proved suitable. Coloproctology service does not suitable for daily using this selection. Even good easy grasping of 4th. By stapler remains difficult definition that fixed externally, so, some prove the using of both stapler and surgery was good results surgery. Good also used in the prolapsing and reducible piles (3rd degree) without any complication.
Conclusion
Both safe with advantage and disadvantage of both for good results and satisfaction with both treatment types. Irrespective of the operative method there is manipulation in painful site. Nearly most patients recure activity without pain after patient’s inspection 3 weeks later. Following the classic Milligan–Morgan-type technique had 6 weeks compared to others methods of improvement median ranged degree of pain and personal self-activity.
References
- Engel AF, Eijsbouts QA (2000) Haemorrhoidectomy: Painful choice. Lancet 355: 2253–2254.
- Macrae HM, Mcleod RS (1995) Comparison of hemorrhoids treatment modalities. A meta-analysis. Dis Colon Rectum 38: 687–694.
[Crossref], [Google scholar], [Indexed]
- Ganio E, Altomare DF, Gabrielli F, Milito G, Canuti S, et al. (2001) Prospective randomized multicentre trial comparing stapled with open haemorrhoidectomy. Br J Surg 88: 669–674.
[Crossref], [Google scholar], [Indexed]
- Hasse C, Sitter H, Brune M, Wollenteit I, Lorenz W, et al. (2004) Haemorrhoidectomy: Conventional exci-sion versus resection with the circular stapler. Prospective, randomized study. Dtsch Med Wochenschr 129: 1611–1617.
[Crossref], [Google scholar], [Indexed]
- Ho YH, Cheong WK, Tsang C (2000) Stapled hemorrhoidectomy–cost and effectiveness. Randomized, controlled trial including incontinence scoring, anorectal manometry and endoanal ultrasound assessments at up to three months. Dis Colon Rectum 43: 1666–1675.
[Crossref], [Google scholar], [Indexed]
- Khalil KH, OBichere A, Sellu D (2000) Randomized clinical trial of sutured versus stapled closed haemorrhoidectomy. Br J Surg 87: 1352–1355.
- Schmidt MP, Fischbein J, Shatavi H (2002) Stapler hemorrhoid-ectomy versus conventional procedures-A clinical study. Zentralbl Chir 127: 15–18.
[Crossref], [Google scholar], [Indexed]
- Kirsch JJ, Staude G, Herold A (2000) Hamorrhoidektomien nach longo trial. Lancet 355: 779–781.
- Shalaby R, Desoky A (2001) Randomized clinical trial of stapled versus Milligan-Morgan haemorrhoidectomy. Br J Surg 88: 1049-1053.
[Crossref], [Google scholar], [Indexed]
- Seow-Choen F (2001) Stapled haemorrhoidectomy: Pain or gain. Br J Surg 88: 1–3.
[Crossref], [Google scholar], [Indexed]
- Chung YC, Wu HJ (2003) Clinical experience of sutureless closed hemorrhoidectomy with LigaSure. Dis Colon Rectum 46: 87–92.
[Crossref], [Google scholar], [Indexed]
- Franklin EJ, Seetharam S, Lowney J, Horgan PG (2003) Randomized, clinical trial of Ligasure vs. conventional diathermy in hemorrhoidectomy. Dis Colon Rectum 46: 1380–1383.
[Crossref], [Google scholar], [Indexed]
- Milito G, Gargiani M, Cortese F (2002) Randomised trial comparing LigaSure haemorrhoidectomy with the diathermy dissection operation. Tech Coloproctol 6: 171–175.
[Crossref], [Google scholar], [Indexed]
- Thorbeck CV, Montes MF (2002) Haemorrhoidectomy: Randomised controlled clinical trial of Ligasure compared with Milligan-Morgan operation. Eur J Surg 168: 482–484.
[Crossref], [Google scholar], [Indexed]
- Kirsch JJ, Staude G, Herold A (2001) Prospektive vergleichsstudie mit 300 Patienten. Chirurg 72: 180–185.
- Rowsell M, Bello M, Hemingway DM (2000) Circumferential mucosectomy (stapled haemorrhoidectomy) versus conventional haemorrhoidectomy: Randomised controlled. Lancet 355: 779-781
[Crossref], [Google scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences